Specific Donor/Recipient HLA Disparities are Associated with Better Long-Term Kidney Allograft Survival among 4-, 5-, and 6-HLA (A/B/DR)-Mismatched Pairs
University of Toledo, Toledo, OH
Meeting: 2019 American Transplant Congress
Abstract number: D360
Keywords: Graft survival, HLA matching, Kidney transplantation
Session Information
Session Name: Poster Session D: Late Breaking
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: The vast majority of deceased donor kidneys are allocated without any consideration for the HLA disparities, which may improve or worsen the survival the post-transplant allograft survival. However specific HLA antigen immunogenicity varies with certain antigen mismatches thought to be protective rather than immunogenic. We performed retrospective analysis of 4-, 5- and 6-HLA (A/B/DR) mismatched pairs to test whether specific HLA-A mismatches may either improve or worsen long-term kidney transplant survival.
*Methods: Cox proportional hazards model (PHR) was built on unadjusted population of 108,975 deceased donor kidney transplants done in 2000-2016 from the SRTR database. Each possible combination of mismatched HLA antigens was considered a covariate in PHR. 15-year graft survival was the outcome variable and best matched (0-HLA mismatches, MM) transplants were analyzed separately from the worst (4-, 5-, or 6-HLA MM) transplants.
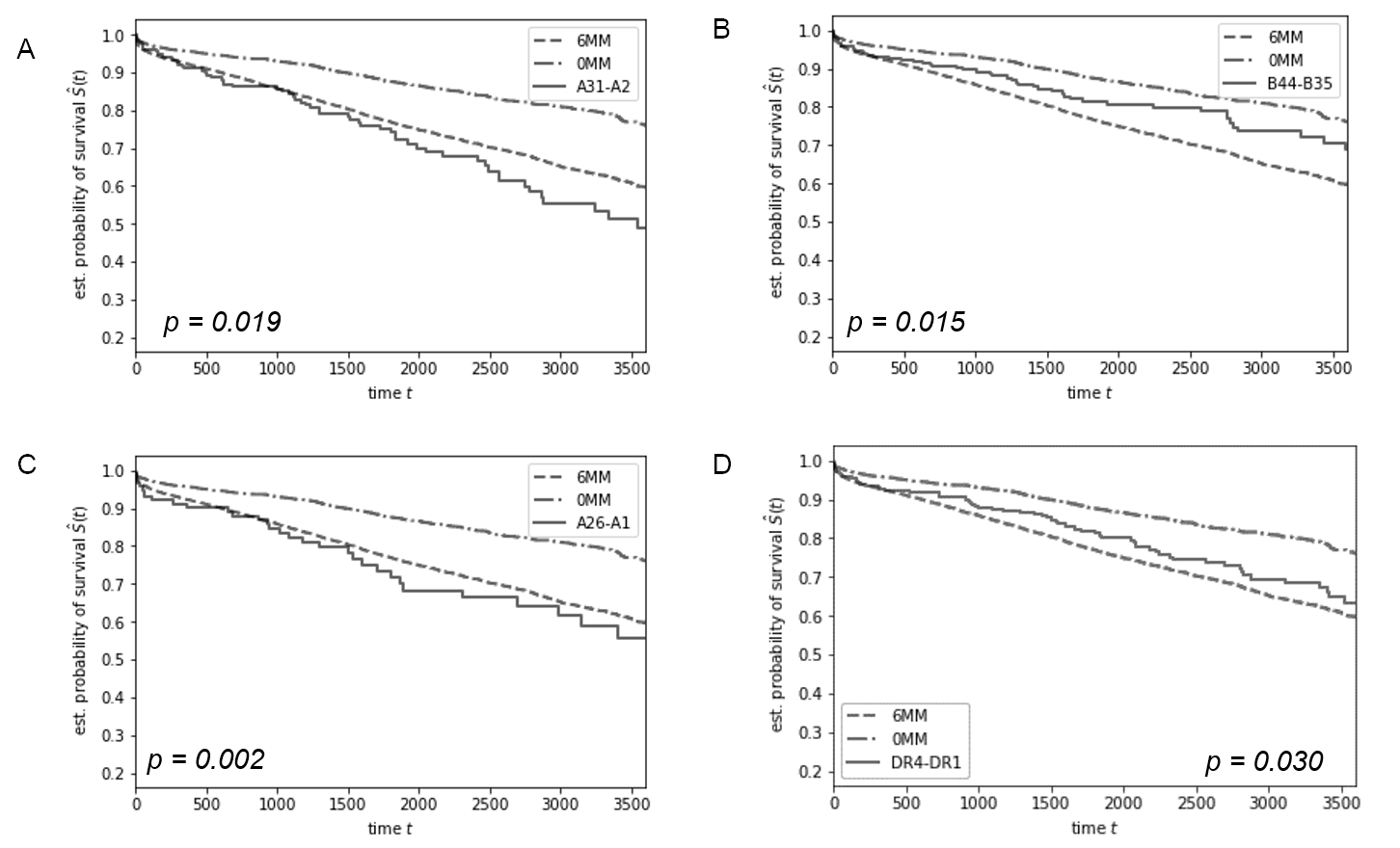
*Results: 30 specific HLA MM (10 HLA-A, 5 HLA-B and 5 HLA-DR) were significantly associated with 15-year graft survival (p<0.05) in transplants with identical number of total HLA MM. As shown in Fig. 1A, 131 pairs with 6 HLA MM, one of which was HLA-A31 donor/HLA-A02 recipient disparity, had significantly worse graft survival compared to other pairs with 6-HLA mismatches (p=0.019). Similarly, 6-HLA mismatched 399 pairs who had HLA-A26 to HLA-A01 disparity showed significantly worse survival compared to the 6-HLA mismatched group (Fig. 1C, p=0.002). In contrast, 82 6-mismatched pairs who had an HLA-B45 to HLA-B35 mismatch had significantly better 15-year graft survival (Fig. 1B, p=0.015), and 399 pairs with 6-HLA mismatches who had HLA-DR4 to HLA-DR1 disparity showed significantly better survival compared to the rest of the 6-HLA mismatched population (Fig. 1D, p=0.03). These observations were confirmed by dividing the 108,975 transplants into training and validation datasets (54,486 and 54,487 pairs), wherein each the 30 established specific antigen mismatches produced similar patterns of survival. Analysis of 4- and 5-HLA mismatched transplants also yielded similar results.
*Conclusions: There are specific HLA-A/B/DR disparities which improve vs. worsen long-term kidney allograft survivals. Selection of these beneficial HLA disparities in clinical programs may dramatically improve kidney allograft survivals among otherwise randomly HLA mismatched pairs.
To cite this abstract in AMA style:
Bekbolsynov D, Zhang H, Mierzejewska B, Rees M, Xu K, Stepkowski S. Specific Donor/Recipient HLA Disparities are Associated with Better Long-Term Kidney Allograft Survival among 4-, 5-, and 6-HLA (A/B/DR)-Mismatched Pairs [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/specific-donor-recipient-hla-disparities-are-associated-with-better-long-term-kidney-allograft-survival-among-4-5-and-6-hla-a-b-dr-mismatched-pairs/. Accessed February 18, 2026.« Back to 2019 American Transplant Congress