Evaluating the Predictive Utility of the Stanford Integrated Psychosocial Assessment for Transplantation (SIPAT) for Post-Transplant Outcomes in Moderate to High-Risk Liver Transplant Candidates
P. Sheiner, S. Spence, D. Gleason, J. Riley, M. Einstein, E. UrtasunSotil, C. Rochon, B. Maneckshana, O. Serrano
Hartford Hospital, Hartford, CT
Meeting: 2019 American Transplant Congress
Abstract number: D312
Keywords: Liver transplantation, Psychosocial
Session Information
Session Name: Poster Session D: Psychosocial and Treatment Adherence
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Previous studies suggest the Stanford Integrated Psychosocial Assessment for Transplantation (SIPAT) is predictive of post-transplant outcomes in multiorgan transplant candidates. We aim to determine the utility of SIPATs in moderate to high risk liver transplant candidates.
*Methods: 168 adult liver transplant candidates with SIPATs reported between January 1st, 2013 and December 31, 2017, were divided based on SIPAT score: low risk (0-20), minimally acceptable (21-39), and high risk (>40). In a retrospective chart review, we documented demographics, SIPAT, transplant status, incidence of rejection, infection, readmissions within one year, mortality and recidivism. Gender, age, ethnicity, insurance, MELD (Model for End-Stage Liver Disease) score, history of substance abuse and hepatocellular carcinoma were collected during pre-transplant evaluation.
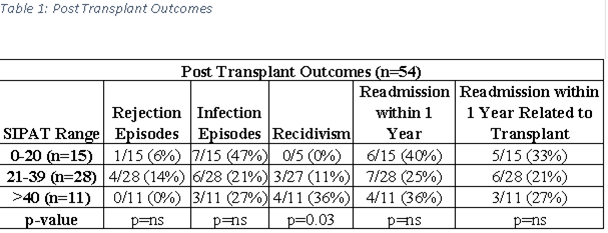
*Results: Of 168 candidates, 70 were listed/transplanted, 98 were not listed. There was a significant difference in mean SIPAT scores who were denied transplant versus those who were listed/transplanted (43±16 vs 31±14, p<0.001).In those patients whose listing was denied, the mortality was 41% vs 11% in those who were listed/transplanted (p<0.001). Fifty-four candidates underwent transplantation: 15 low risk, 28 minimally acceptable, and 11 high risk. No difference was seen in the transplant outcomes of incidence of rejection, infection, readmissions within one year and mortality(table 1).Mean SIPAT score correlated with type of insurer. Higher scores associated with Medicaid-a surrogate for poorer socioeconomic status(p<0.03): 43/54 candidates had a history of substance abuse, with 7/43 (16%) experiencing recidivism. No significance was evident when comparing mean SIPAT of individuals with recidivism and those without (48±18 vs 34 ±13); however, there was when contrasting recidivism of candidates with SIPATs <40 and SIPATs >40 (7/36 vs 4/7; p<0.003).
*Conclusions: The SIPAT is not predictive of most post-transplant outcomes in moderate to high risk liver transplant candidates but there was a significant increase in recidivism in high risk patient. The SIPAT is still useful as a screening tool to mitigate psychosocial risk factors prior to transplantation
To cite this abstract in AMA style:
Sheiner P, Spence S, Gleason D, Riley J, Einstein M, UrtasunSotil E, Rochon C, Maneckshana B, Serrano O. Evaluating the Predictive Utility of the Stanford Integrated Psychosocial Assessment for Transplantation (SIPAT) for Post-Transplant Outcomes in Moderate to High-Risk Liver Transplant Candidates [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/evaluating-the-predictive-utility-of-the-stanford-integrated-psychosocial-assessment-for-transplantation-sipat-for-post-transplant-outcomes-in-moderate-to-high-risk-liver-transplant-candidates/. Accessed February 23, 2026.« Back to 2019 American Transplant Congress