Gender Disparities In Cirrhosis: New Findings In A Large Pretransplant Population
Northwestern Memorial Hospital, Chicago, IL
Meeting: 2019 American Transplant Congress
Abstract number: C292
Keywords: Allocation, Liver cirrhosis, Multicenter studies, Resource utilization
Session Information
Session Name: Poster Session C: Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Type: Poster Session
Date: Monday, June 3, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: There is concern that female patients may suffer worse outcomes than their male counterparts while awaiting liver transplant. Studies on this topic often use databases of listed patients which may introduce selection bias. We therefore analyzed a large, city wide sample of pre-referral patients to assess if disparities exist prior to listing.
*Methods: We utilized HealthLNK, a Chicago-wide database that incorporates the de-identified electronic medical records from six major health care institutions. We included adult patients with ICD-9 codes of cirrhosis who were not on Coumadin during the period of January 1, 2006, and December 31, 2012. We linked patient records with the state death registry and classified patients’ death certificates as “liver related”, “non-liver related”, and “non-descript”. “Liver-Related” mortality was used as the primary outcome for survival analysis. Time at risk was defined as time from inclusion to either death or transplant with censoring at the end of the study. Chi-squared tests, t-tests, and Cox regression were used for statistical inference.
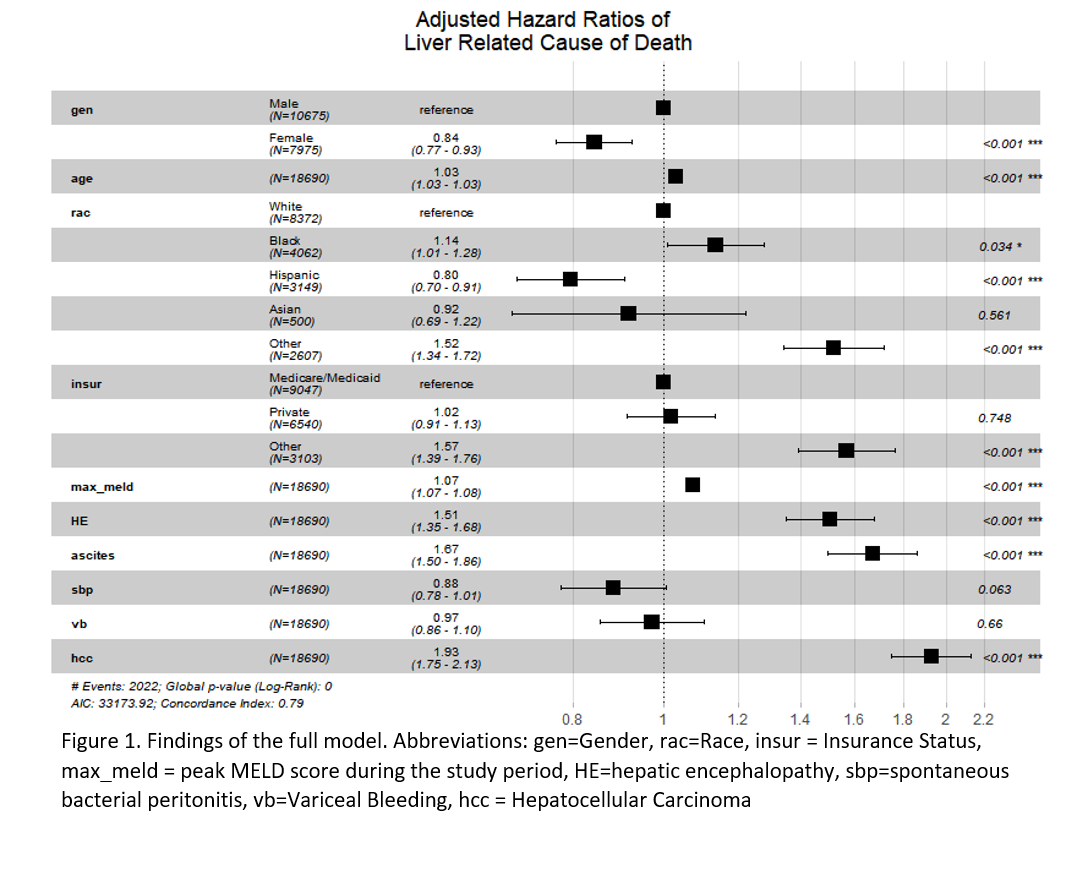
*Results: Out of 18,690 patients included, 7,975 (42.6%) were female. Both male and female patients had similar distributions of age, race, insurance status, and non-hepatic comorbidities as measured by the Elixhauser co-morbidity index. The most common etiologies of liver disease in both men and women were related to HCV, NASH, and Alcohol, however women had more cholestatic liver disease (17% vs 6% in men p<0.001). Women were less likely to have decompensated cirrhosis with lower rates of ascites (31% vs 37%, p<0.001), encephalopathy (28% vs 32%, p<0.001), variceal bleeding (7% vs 10%, p<0.001), hepatocellular carcinoma (10% vs 17%, p<0.001) and spontaneous bacterial peritonitis (5% vs 7%, p<0.001). In concordance with the pre-referral nature of the cohort, 4% of patients underwent transplant and 50% of patients had appropriate labs from which a MELD score could be generated. Women had a lower peak-MELD (15.6 vs 17.3, p<0.001) and were less likely to receive transplants (3.2% vs 4.9%, p<0.001). However in univariate survival analysis, female sex conferred a protective effect with a 30% decrease in the hazard of liver related death (HR 0.70 95% CI 0.65—0.75, p<0.001). After adjustment for multiple confounders female sex was still associated with a decrease of 16% in the hazard of liver related death as illustrated in Figure 1.
*Conclusions: In summary, in this pre-referral cohort we found female patients were less likely to receive transplants but overall had a lower rate of liver related mortality.
To cite this abstract in AMA style:
Mazumder N, Atiemo K, Daud A, Zhao L, Abecassis M, Levitsky J, Ladner DP. Gender Disparities In Cirrhosis: New Findings In A Large Pretransplant Population [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/gender-disparities-in-cirrhosis-new-findings-in-a-large-pretransplant-population/. Accessed March 3, 2026.« Back to 2019 American Transplant Congress