The Liver Frailty Index is Associated with Current and Subsequent Disability in Liver Transplant Candidates
University of California, San Francisco, San Francisco, CA
Meeting: 2019 American Transplant Congress
Abstract number: A314
Keywords: Liver cirrhosis, Liver transplantation, Outpatients, Survival
Session Information
Session Name: Poster Session A: Liver: Recipient Selection
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: The Liver Frailty Index (LFI) was developed to capture the effects of malnutrition and muscle wasting in patients with cirrhosis awaiting liver transplantation (LT). While the LFI consists of measurement of grip strength, chair stands, and balance, little is known of its relationship with disability, a more patient oriented outcome.
*Methods: Included were consecutive adult LT candidates listed at one center who underwent outpatient testing of frailty using LFI (grip, chair stands, balance) and disability using Activities of Daily Living (ADL; range 0-6) and Instrumental ADL (IADL; range 0-8) scales. Frailty was categorized as robust, less robust, pre-frail, and frail using LFI cut-points <3.2, 3.2-3.7, 3.8-4.4, and ≥4.5. Using the p test of trend, we compared: 1) rates of disability (=ADL<6 or IADL<8) at baseline by LFI category for all patients and 2) rates of worsening disability (=ADL or IADL score worse than baseline) among those with ≥2 assessments (n=587). We used multilevel logistic mixed effects regression to associate LFI with: 1) current disability (defined as ADL<6 or IADL<8) and 2) incident disability at 6 +/- 2 months among those with no disability at baseline.
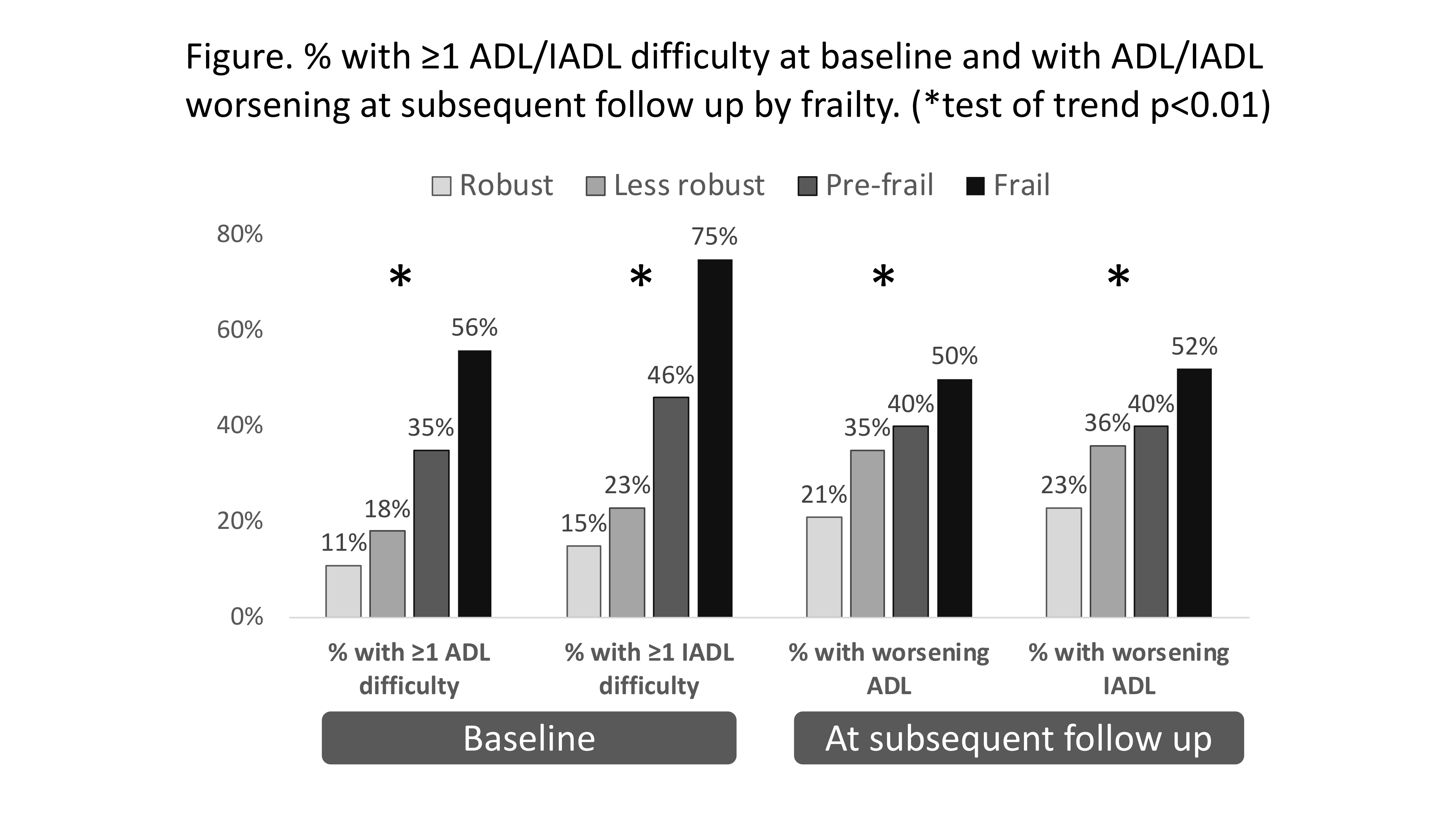
*Results: Of 983 LT candidates, median [interquartile range (IQR)] baseline LFI was 3.8 (3.3-4.2): 20% were robust, 32% less robust, 33% pre-frail, 15% frail. At baseline, higher LFI categories were associated with a greater % with ≥1 ADL or IADL difficulty [Fig]. A total of 587 (60%) had ≥1 assessment. Higher LFI categories were associated with subsequent worsening of disability [Fig]. In multilevel mixed models adjusted for MELD, encephalopathy, ascites, gender, age, and time, each point increase in LFI was associated with 3.4 and 4.8 higher odds of current difficulty with ≥1 ADL (95%CI 2.7-4.2) and ≥1 IADL (95%CI 3.7-6.2) [p<0.001 for each], respectively . Among patients without disability at baseline (ADL n=294, IADL n=265), each point increase in LFI was associated with 2.8 and 1.6 higher odds of having difficulty with ≥1 ADL (95%CI 1.6-5.1, p=0.001) and ≥1 IADL (95%CI 1.0-2.7, p=0.05) at 6 months.
*Conclusions: LFI – an objective, low-cost, clinic-based metric – is strongly associated with concurrent, incident, and worsening disability in patients with cirrhosis. In the clinic setting, the LFI can be used to identify those in greatest need for additional support / resources to maintain functional independence. In the research setting, the LFI may help select for an enriched population for clinical trials of interventions aimed at improving functional status and quality of life.
To cite this abstract in AMA style:
Lai JC, Dodge JL, McCulloch CE, Covinsky KE, Singer JP. The Liver Frailty Index is Associated with Current and Subsequent Disability in Liver Transplant Candidates [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/the-liver-frailty-index-is-associated-with-current-and-subsequent-disability-in-liver-transplant-candidates/. Accessed February 22, 2026.« Back to 2019 American Transplant Congress