Efficacy of Belatacept Conversion Protocols
Kaiser Los Angeles Medical Center, Los Angeles, CA
Meeting: 2019 American Transplant Congress
Abstract number: A227
Keywords: Calcineurin, Co-stimulation, Immunosuppression, Rejection
Session Information
Session Name: Poster Session A: Kidney Immunosuppression: Novel Regimens and Drug Minimization
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Belatacept (bela) is approved for de novo use in kidney transplantation. Conversion from CNI to bela is utilized for various reasons. Conversion is off-label and there is no standard protocol. We aim to explore the efficacy of conversion protocols used by transplant centers that serve the Southern California Kaiser Permanente population.
*Methods: All patients converted to bela were initially included in this retrospective chart review. The primary outcome was rejection. Secondary outcomes were graft and patient survival, creatinine (Cr) change, infection, DSA, and PTLD. Maintenance immunosuppression was also recorded before and after conversion. Continuous variables were reported as a median [IQ Range] and categorical variables as a frequency (%).
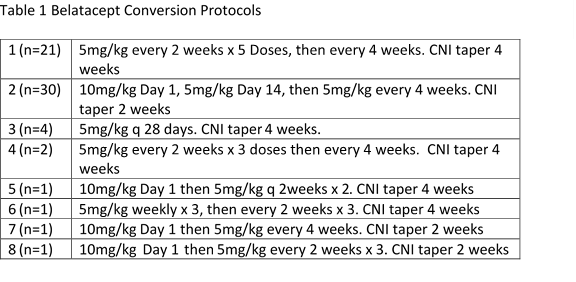
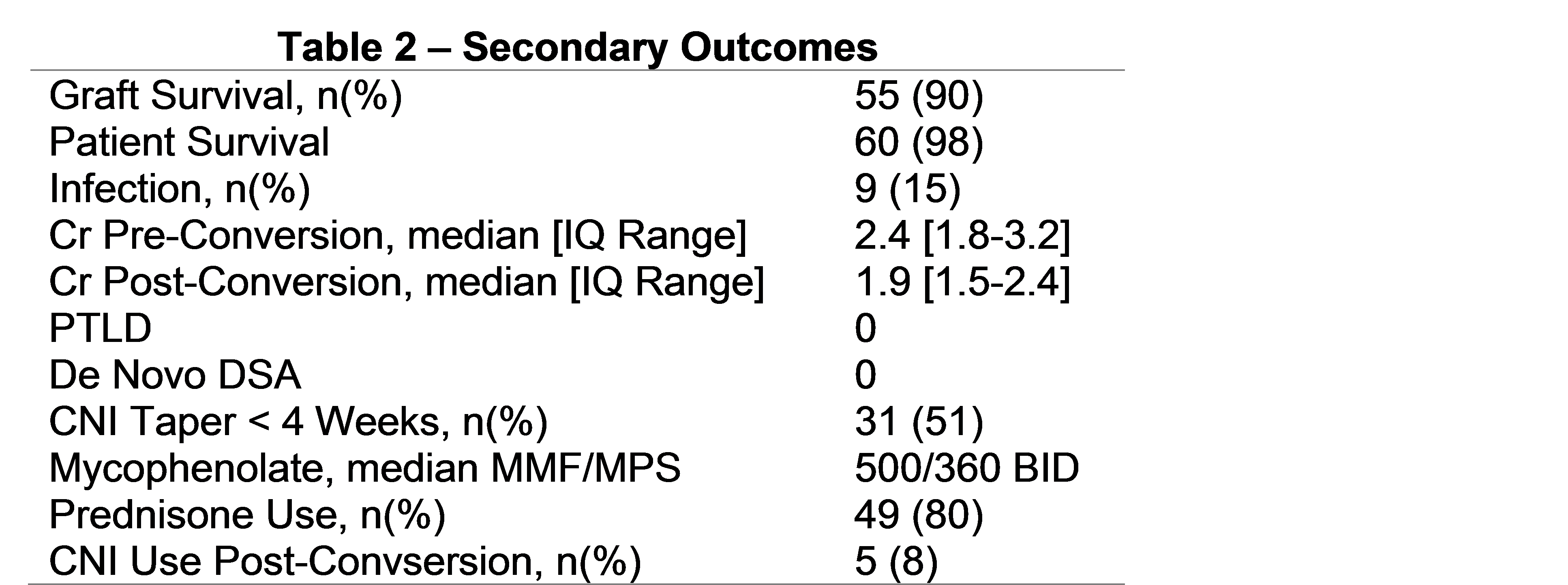
*Results: Eight different conversion protocols were identified in 61 patients transplanted at 5 different centers (Table 1). Time to conversion was 290 [90-642] days post transplant with 277 [123-1539] days of follow-up post conversion. 79% had a deceased donor. Cr prior to switch was 2.4 [1.8-3.2]. The most common reasons for switch were CNI toxicity (n=20), IFTA (n=19), and ATN/DGF (n=17). Other reasons included TMA and drug intolerance. There were 2 (3%) rejections within 6 months of conversion (both < 90 days). None of these patients lost their allograft. There were no observed differences in rejection when comparing Protocol 1 and 2 and the CNI taper regimens. Those in protocol 2 were converted later compared to protocol 1 (p=.001). Secondary outcomes are seen in Table 2. Cr improved by 0.5mg/dl. 5/6 graft losses were within 1 year of conversion. Those with graft failure had a higher Cr, KDPI and were converted later post transplant. There were 9 infections within 6 months of conversion (1 BK, 1 CMV). 1 death was related to sepsis 2 years after conversion. 9 (15%) had DSA pre-conversion. There was no de novo DSA or change in MFI post-conversion.
*Conclusions: We found a variety of conversion protocols utilized at different transplant centers in this sizable cohort. There were no observed differences in the protocols with regards to outcomes. A higher Cr at time of conversion was associated with allograft loss. A less intense bela conversion protocol with a 4 week CNI taper may be appropriate. Larger studies are need to determine the best strategy.
To cite this abstract in AMA style:
Yazdi M, Kahwaji J, Meguerditchian S, Lee R. Efficacy of Belatacept Conversion Protocols [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/efficacy-of-belatacept-conversion-protocols/. Accessed March 5, 2026.« Back to 2019 American Transplant Congress