Beta2-Adrenergic Receptor Activation Prolongs Survival of Vascularized Composite Tissue Allotransplants in a Murine Model
1Surgical Oncology, Roswell Park Comprehensive Cancer Center, Buffalo, NY, 2Pathology, Roswell Park Comprehensive Cancer Center, Buffalo, NY, 3Cardiology, University at Buffalo, Buffalo, NY, 4Immunology, Roswell Park Comprehensive Cancer Center, Buffalo, NY
Meeting: 2019 American Transplant Congress
Abstract number: A61
Keywords: Immunosuppression, T cell activation
Session Information
Session Name: Poster Session A: Basic & Clinical Science – VCA
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Transplantation of faces, hands, and limbs using vascularized composite allotransplantation (VCA) has faced significant challenges hindering its routine implementation in the clinic. One critical hurdle is the scarcity of adequately matched HLA donors, resulting in high doses of immunosuppressants which present significant risks to the patient. Alternative methods of controlling rejection are desperately needed. One possibility could be in exploiting the links between the nervous and immune systems that regulate host defense and responses to stress. The neurotransmitter norepinephrine regulates immune cells, acting via the β-adrenergic receptor (β2-AR). Based upon data by our lab showing the role of β2-AR signaling for decreasing graft-versus-host disease following bone marrow transplantation, we hypothesized that β2-AR activation using the drug terbutaline would suppress immune cell function without the harmful side effects of toxic immunosuppressive drugs in the setting of HLA-mismatched VCA.
*Methods: Heterotopic hind limb transplantation mouse model of VCA was used with C57BL/6 (H-2b) as recipients and BALB/c (H-2d) mice as donors. Graft survival was tested with daily terbutaline injections. Different regimens of tacrolimus and terbutaline were investigated as a salvage treatment.
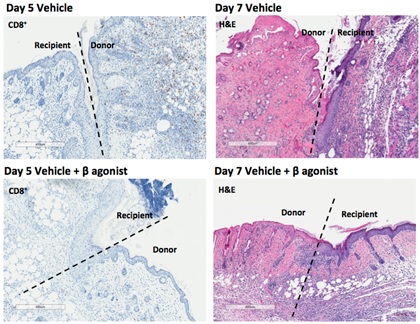
*Results: Even though terbutaline did not completely protect transplanted grafts from rejection there were fewer CD4+/8+ effector T cells infiltrating the graft site, delayed graft rejection, and lower histologic and gross rejection grades without severe side effects. A significant reduction was noted in IFNγ secreting CD4 T cells in the terbutaline group compared to the vehicle group. Additionally, in the salvage therapy tests terbutaline itself maintained grafts without severe rejection for a longer period than vehicle after stopping tacrolimus. Mechanistically, β-AR agonist inhibited T-cell activation by suppressing glucose uptake via GLUT1 channel delaying the immune response.
*Conclusions: Encouragingly, β2-AR agonist could decrease doses of toxic immunosuppressive drugs to maintain healthy grafts, and may serve as a bridging therapy while recipients cannot take immunosuppressive drugs due to toxicities. Further investigations are needed to maximize the efficacy of β2-AR agonist in transplant immunosuppression.
To cite this abstract in AMA style:
Kim M, Fisher D, Loo J, Bogner P, Sharma U, Skitzki J, Repasky E. Beta2-Adrenergic Receptor Activation Prolongs Survival of Vascularized Composite Tissue Allotransplants in a Murine Model [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/beta2-adrenergic-receptor-activation-prolongs-survival-of-vascularized-composite-tissue-allotransplants-in-a-murine-model/. Accessed March 7, 2026.« Back to 2019 American Transplant Congress