Improving the Organ Donation Process: Updated
J. Yeh, M. P. Jarrett, L. Teperman
Northwell Health, New Hyde Park, NY
Meeting: 2019 American Transplant Congress
Abstract number: 612
Keywords: Donors, unrelated, Efficacy, Outcome, Resource utilization
Session Information
Session Name: Concurrent Session: Quality Assurance Process Improvement & Regulatory Issues II
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:42pm-5:54pm
Presentation Time: 5:42pm-5:54pm
Location: Room 210
*Purpose: Due to the complexity of care that each ICU patient requires, the bedside nurse may miss the clinical trigger that would indicate an appropriate referral to the OPO, resulting in a missed or a late referral. Timely referrals, referrals made within 1 hour of meeting clinical triggers, by the care team allow the OPO adequate time to thoroughly review the patient’s medical chart and collaborate with the critical care team to optimize donation opportunities. By utilizing the nurses in the Tele-ICU, we found a way to give back time to the clinicians at the bedside, increase the number of referrals made, and improve the timeliness of those referrals. This abstract contains an updated pre- and post- study implementation analysis.
*Methods: Through Tele-health technology, a specially trained critical care team monitors patients and their care from an off-site location. This team serves as an extra layer of support and a second set of eyes to the bedside healthcare team. The eICU nurses are critical care trained nurses that have been trained to respond to data driven alerts. In collaboration with our local OPO, the eICU nursing staff conducted a 2 month blind study where eICU nurses were trained to identify patients who met clinical triggers while the bedside team continued to make the referrals as they normally would.
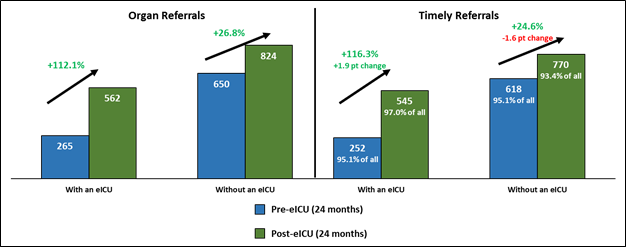
*Results: During the initial blind study, the eICU nurses identified all the patients for whom actual referrals were made by the hospital staff. In addition, the eICU nurses appropriately identified 5.5 times more referrals than the ones called in to the OPO from the hospital care team. Of the actual referrals made by the hospital staff, 76.5% of them were identified earlier by the eICU nurses than by the bedside team. Due to the compelling data, the organ donation referral process was officially implemented for real-time use at 5 hospitals. In an expanded study to review the efficacy of the intervention, we compared referral data 24 months pre- and post- implementation. The number of organ donor referrals increased by 112.1% in ICU’s with eICU capability and the percent of timely referrals rose from 95.1% to 97.0%. In comparison, the ICU’s without the eICU function increased the number of organ referrals by 26.8%, however the percent of timely referrals fell from 95.1% to 93.4%.
*Conclusions: By evaluating our current workflows in the ICU and Tele-ICU, we were able to enhance the already existing eICU Monitoring Program to include the organ donation referral process. In doing so, we were able to significantly improve the number and the timeliness of organ referrals to our OPO. Accurate and timely referrals help maintain donation as an option for all potential patients.
To cite this abstract in AMA style:
Yeh J, Jarrett MP, Teperman L. Improving the Organ Donation Process: Updated [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/improving-the-organ-donation-process-updated/. Accessed February 13, 2026.« Back to 2019 American Transplant Congress