Impact Of Subclinical Bk Virus-associated Nephropathy In High-risk Recipients
University of Alabama, Birmingham, AL
Meeting: 2019 American Transplant Congress
Abstract number: 530
Keywords: Outcome, Polyma virus, Protocol biopsy
Session Information
Session Name: Concurrent Session: Kidney: Polyoma
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:42pm-4:54pm
Presentation Time: 4:42pm-4:54pm
Location: Ballroom B
*Purpose: BK virus-associated nephropathy (BKVAN) is a major contributor to kidney transplant failure. Surveillance of serum and urine for the BKV genome has been incorporated in many programs to subvert development of BKVAN. Surveillance biopsies can detect subclinical (SC)-BKVAN in patients with BK viremia prior to clinical dysfunction. Previous studies have reported better outcomes in SC-BKVAN compared to BKVAN with allograft dysfunction, but in homogeneous cohorts with low immunologic risk. The purpose of this study was to define the incidence and impact of SC-BKVAN on kidney transplant outcomes in a heterogeneous cohort with increased immunologic risk.
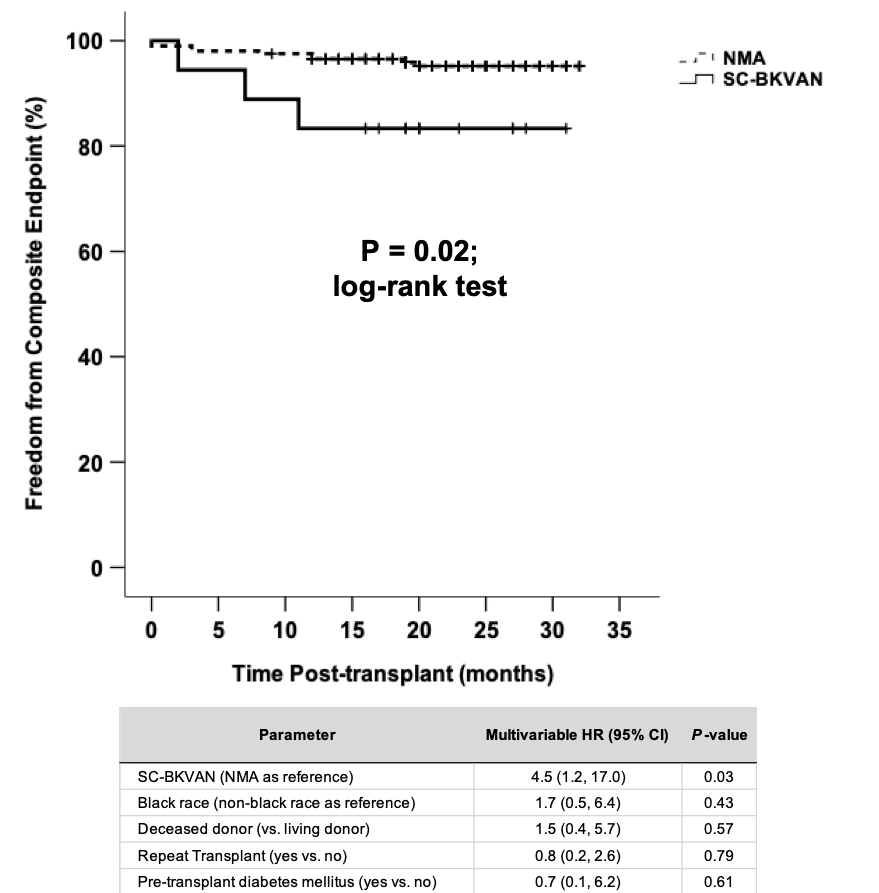
*Methods: We performed a nested case-control study (n=221) within a cohort of 302 kidney recipients with 6-month surveillance biopsies between May 2015 and December 2017. The primary exposure was SC-BKVAN, defined as positive immunohistochemistry for SV40 large T antigen in a 6-month surveillance biopsy without overt clinical dysfunction. The primary outcome was a composite endpoint of acute rejection or death-censored graft loss by 3 years. We examined the effect of SC-BKVAN on the composite endpoint using Kaplan-Meier methods and adjusted for clinical covariates using Cox regression.
*Results: We detected SC-BKVAN in 18/302 (6%) of our parent surveillance cohort. For our nested case-control study, we compared all cases with SC-BKVAN (n=18) to all controls with no major abnormalities (NMA; n=203). Our cohort was enriched for increased immunologic risk, including 61% deceased donor type, 55% black race, 52% glomerular/diabetic cause of end-stage kidney disease, and 11% repeat transplants. SC-BKVAN was associated with concurrent subclinical inflammation in 17/18 (94%) cases, including borderline changes (n=11), T cell-mediated rejection (n=5), and antibody-mediated rejection (n=1). Compared to NMA, SC-BKVAN had higher Banff acute injury scores (P ≤ 0.001 for tubulitis, endarteritis, and interstitial inflammation) but similar chronic injury scores. SC-BKVAN was associated with over 4-fold increased hazard for the composite endpoint after adjustment for race, donor type, repeat transplant, and pre-transplant diabetes.
*Conclusions: We detected SC-BKVAN in 6% of high-risk recipients at 6 months post-transplant, much higher than previously reported in lower risk cohorts. SC-BKVAN was associated with subclinical inflammation and inferior 3-year outcomes. This study illustrates the importance of underlying immunologic risk on the impact of subclinical BKV infection.
To cite this abstract in AMA style:
Seifert ME, Kasik EP, Bernard M, Agarwal G, Fatima H, Gaston R, Julian B, Kew C, Kumar V, Mehta S, Ong S, Rosenblum F, Towns G, Mannon RB. Impact Of Subclinical Bk Virus-associated Nephropathy In High-risk Recipients [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-subclinical-bk-virus-associated-nephropathy-in-high-risk-recipients/. Accessed January 4, 2026.« Back to 2019 American Transplant Congress