Use of Marginal Liver Donors in Pediatric Transplantation: Diverse Profiles of Use in Major Transplant Centers
1Surgery, UT Southwestern, Dallas, TX, 2Pediatrics, UT Southwestern, Dallas, TX, 3Medicine, UT Southwestern, Dallas, TX
Meeting: 2019 American Transplant Congress
Abstract number: 494
Keywords: Donors, marginal, Liver, Liver grafts, Pediatric
Session Information
Session Name: Concurrent Session: Liver: Pediatrics
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:30pm-2:42pm
Presentation Time: 2:30pm-2:42pm
Location: Room 210
*Purpose: Pediatric liver transplantation is highly specialized only a small number of centers have consistent large volume experience. We tested the hypothesis that large volume pediatric liver transplant centers would show patterns of increased use of marginal livers compared with other pediatric transplant centers.
*Methods: The Scientific Registry of Transplant Recipients (SRTR) database was used to examine outcomes in all patients who had undergone liver transplantation between 2000 to 2018. Pediatric patients, defined as < 18 years, were identified. We identified high volume pediatric centers as a center that has performed >20 livers in 2017 and historically >200 liver transplants. Marginal livers were defined as: donation after cardiac (DCD), donor age > 45 years; donor livers with terminal transaminases > 500 units per liter; cold ischemic time of allograft > 10 hours; distance to donor center of > 500 miles; a regional or national shared liver; donor having been hospitalized in the ICU for > 1 week prior to procurement; a donor liver with biopsy-proven macrosteatosis >5%; or donor serologies positive for hepatitis B core antibody or hepatitis C. A p-value of <0.05 was considered significant.
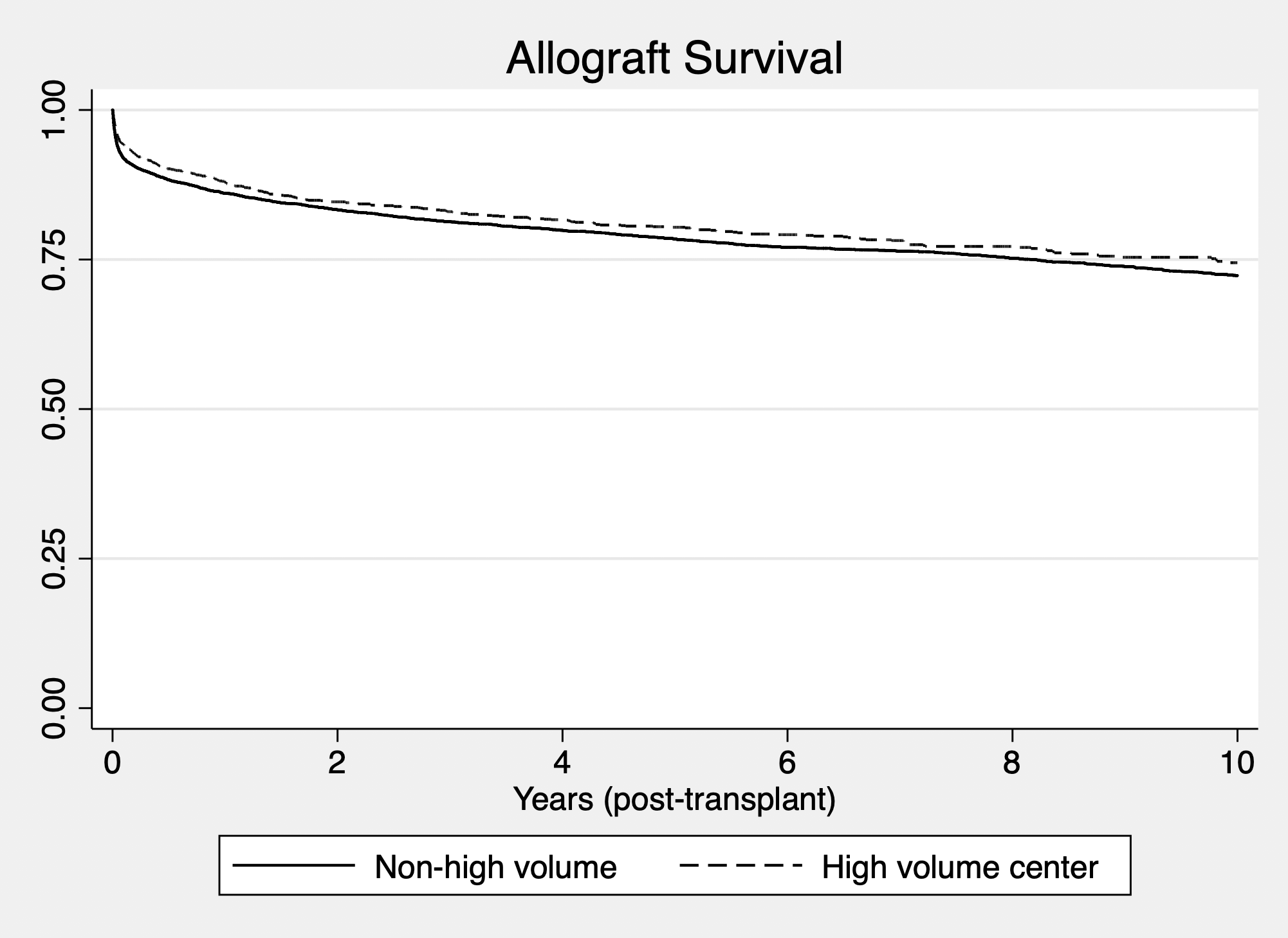
*Results: Six centers fulfilled criteria for major pediatric liver transplant center. Analysed together these centers used more regionally shared liver vs. other centers (51% vs. 40%, p < 0.05) and had a longer distance to travel for donors (29.6% vs. 20.2%, p < 0.05), but less likely to use a donor > 45 years (1.55% vs. 3.23%, p < 0.05) or a donor in the ICU over one week (32.3% vs. 42.4%, p < 0.05). No significant differences between the two groups in the other marginal factors. Examining each major center individually, each center had increased utilization in a different, single type of marginal liver allograft. Long-term overall allograft survival at major centers compared with all other centers was superior (p < 0.05).
*Conclusions: Use of marginal livers varies across the major pediatric centers. Each center has focused its efforts on maximizing use of a specific type of marginal allograft, and no center had universal experience in utilization of all marginal allografts. Dissemination of experiences from individual sites and strategies to optimize use of marginal livers could lead to enhanced utilization and outcomes nationwide.
To cite this abstract in AMA style:
Hwang CS, Aqul A, Mufti A, Hanish S, Desai D, Vagefi P, MacConmara M. Use of Marginal Liver Donors in Pediatric Transplantation: Diverse Profiles of Use in Major Transplant Centers [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/use-of-marginal-liver-donors-in-pediatric-transplantation-diverse-profiles-of-use-in-major-transplant-centers/. Accessed February 20, 2026.« Back to 2019 American Transplant Congress