Access To The Kidney Transplant Waitlist For Patients With Hiv And End-stage Renal Disease
A. A. Shaffer1, H. Ying2, N. Chu1, A. G. Thomas3, C. Haugen2, S. Norman4, D. L. Segev1, M. A. McAdams-DeMarco1
1Surgery & Epidemiology, Johns Hopkins University, Baltimore, MD, 2Surgery, Johns Hopkins University, Baltimore, MD, 3Epidemiology, University of North Carolina, Chapel Hill, NC, 4Surgery, University of Michigan, Ann Arbor, MI
Meeting: 2019 American Transplant Congress
Abstract number: 443
Keywords: HIV virus, Kidney transplantation, Multicenter studies, Waiting lists
Session Information
Session Name: Concurrent Session: Kidney Psychosocial II: Substances and Access & Barriers
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:30pm-3:42pm
Presentation Time: 3:30pm-3:42pm
Location: Room 302
*Purpose: Patients with HIV and end-stage renal disease (ESRD) experience higher mortality on dialysis than those without HIV. These HIV+ dialysis patients may face barriers to kidney transplantation (KT) that result from delayed referrals or factors identified at the time of evaluation.
*Methods: We used a prospective, longitudinal multi-center cohort to study 98 HIV+ and 3,105 HIV- patients with ESRD who were evaluated for KT between 2008 and 2017. We compared patient characteristics using rank-sum (for continuous variables) and Fisher’s exact (for categorical variables) tests and estimated the likelihood of listing by HIV-status using Kaplan-Meier plots with the log-rank test and adjusted Cox regression. The presence of comorbidities was defined as a Charlson comorbidity index (CCI) score ≥1; cognitive impairment was defined as a mini-mental state exam score ≤80.
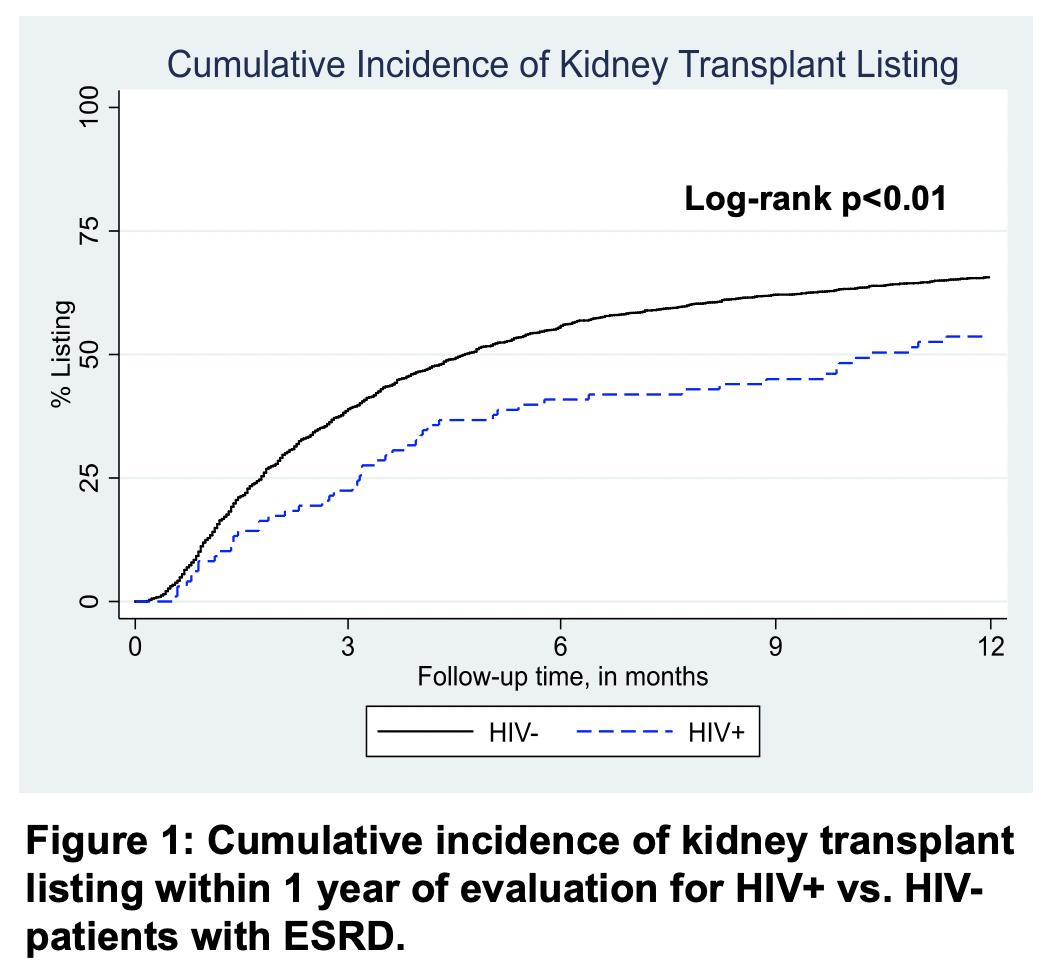
*Results: Patients with HIV (3.1%) were more often young (median 54 vs. 56 years old), African American (91 vs. 43%), men (72 vs. 59%), with cognitive impairment (15 vs. 6%), and longer time on dialysis prior to KT evaluation (median 2.4 vs. 1.3 years) than those without HIV. Within 1 year of KT evaluation, 52 HIV+ and 2,010 HIV- patients were listed for KT; median time from evaluation to listing was 133 days for HIV- patients and 315 days for HIV+ patients (Figure 1).
Adjusting for age, gender, African American race, comorbidities, and cognitive impairment, patients with HIV were less likely to be listed (aHR: 0.70, 95%CI: 0.52-0.93; p<0.05). However, additionally adjusting for time on dialysis attenuated this difference (aHR: 0.90, 95%CI: 0.67-1.20; p=0.5) (Table 1).
| Hazard Ratio | 95% CI | p-value | |
| HIV- | Reference | ||
| HIV+ (Unadjusted) | 0.68 | 0.52-0.90 | <0.01 |
| HIV+ (Adjusted) | 0.69 | 0.52-0.93 | <0.05 |
| HIV+ (Further Adjusted for Dialysis Time) | 0.92 | 0.69-1.20 | 0.6 |
*Conclusions: HIV+ patients have a lower likelihood of KT listing that is not explained by differences in patients’ characteristics other than time on dialysis prior to evaluation. Targeted dialysis interventions for early referral and transplant evaluation may improve access to KT for HIV+ patients with ESRD.
To cite this abstract in AMA style:
Shaffer AA, Ying H, Chu N, Thomas AG, Haugen C, Norman S, Segev DL, McAdams-DeMarco MA. Access To The Kidney Transplant Waitlist For Patients With Hiv And End-stage Renal Disease [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/access-to-the-kidney-transplant-waitlist-for-patients-with-hiv-and-end-stage-renal-disease/. Accessed February 28, 2026.« Back to 2019 American Transplant Congress