Impact of Coronary Artery Disease on Long-Term Mortality after Liver Transplantation
1Division of Gastroenterology, Hepatology and Nutrition, Department of Internal Medicine, Virginia Commonwealth University, Richmond, VA, 2Department of Bio-statistics, Virginia Commonwealth University, Richmond, VA, 3Virginia Commonwealth University, Richmond, VA, 4Department of Internal Medicine, Virginia Commonwealth University, Richmond, VA, 5Department of Transplant Surgery, Virginia Commonwealth University, Richmond, VA
Meeting: 2019 American Transplant Congress
Abstract number: 437
Keywords: Liver transplantation, Survival
Session Information
Session Name: Concurrent Session: Liver Transplant Complications and Retransplantation II
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:42pm-3:54pm
Presentation Time: 3:42pm-3:54pm
Location: Ballroom A
*Purpose: Cardiovascular disease (CVD) is an important cause of post liver transplantation (LT) mortality and is higher than age-and gender matched cohorts. This happens despite careful pre-LT selection where patients deemed to be high risk for CVD are excluded from LT consideration. Thus, the key driver of this post-LT mortality is not known. We hypothesized that patients after LT have accelerated atherosclerosis and therefore, pre-LT coronary artery disease (CAD) would not be able to predict overall and CVD associated mortality post-LT.
*Methods: Protocol coronary angiography is performed in all patients aged >50 years or risk factors (diabetes, hypertension, obesity, family history, smoking history) prior to LT. Those without risk factors and <50 years old have non-invasive cardiac stress test and coronary angiography was limited to those with positive stress test. All adult patients receiving LT from 1/2007 to 1/2017 were included (N=495). The primary and secondary outcomes were all cause mortality and CVD mortality, respectively. A Cox proportional hazards model was conducted on survival after LT adjusting for age, etiology of chronic liver disease, CAD, smoking, and diabetes.
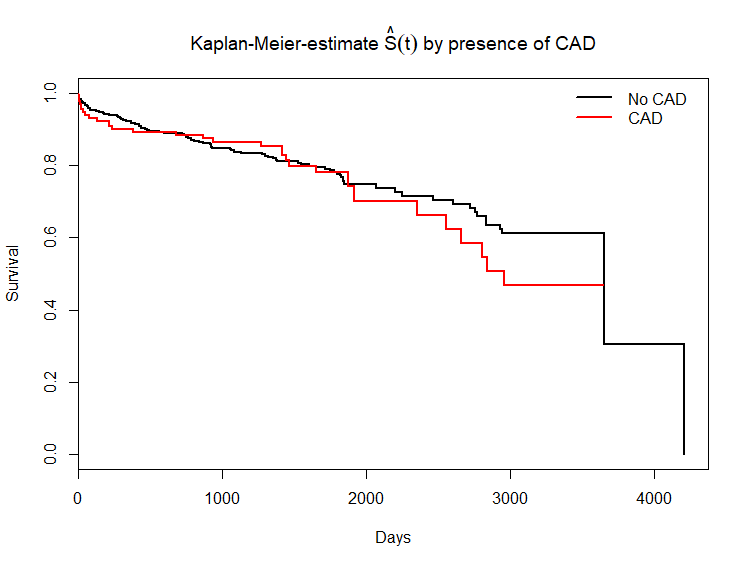
*Results: A total of 495 LTR were enrolled. The mean age of the LT recipients (LTR) was 55 ± 9 years and 358 (72%) were males. The prevalence of CAD as noted on angiography was 26% prior to LT. After median follow up of 4.5 years (range:0-11 years), 120 (24.2%) deaths occurred, 29 (5.9%) of which were related to CVD. The 1-, 3- and 5-year survival rates were 91.5%, 84.4%, and 75.4%%, respectively. The overall mortality rates were similar between those with and without CAD at baseline (Figure 1). No association between presence, severity or history of CAD intervention with overall mortality was found. The etiology of liver disease was not related to overall mortality (Table 1). While NASH is closely associated with CAD (38.5% vs. 23.7% p=0.009), in sub-group analysis CAD did not impact survival in patients transplanted for NASH cirrhosis [HR:1.47, 95%CI:0.47, 4.62].
*Conclusions: Despite aggressive attempts to risk stratify patients prior to LT, cardiovascular risk is not fully captured on pre-LT cardiac evaluation, lending further support to factors that are exacerbated post-LT. More importantly the prevalence of CVD mortality post-LT was much higher than the reported general population suggesting potential limitation in clinical management that need to be overcome if we are to improve long-term survival in LTR.
| Characteristics | Hazard Ratio (95% CI) | p-values |
| CAD present | 1.00 (0.66, 1.53) | 0.972 |
| NASH | 0.65 (0.37, 1.14) | 0.131 |
| Age | 1.03 (1.00, 1.05) | 0.034 |
| Smoking | 1.36 (0.94, 1.97) | 0.106 |
| Diabetes | 1.37 (0.93, 2.02) | 0.111 |
To cite this abstract in AMA style:
Patel SS, Rodriguez VA, Siddiqui MB, Laurenzano J, Lin F, Clinton J, Faridnia M, Chandrakumaran A, Reichman T, Bhati C, Siddiqui MS. Impact of Coronary Artery Disease on Long-Term Mortality after Liver Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-coronary-artery-disease-on-long-term-mortality-after-liver-transplantation/. Accessed January 14, 2026.« Back to 2019 American Transplant Congress