Factors Associated with Cardiovascular Subclinical Target Organ Damage in Liver Transplant Recipients
1Department of Pediatric Kidney, Liver, and Metabolic Diseases, Hannover Medical School, Hannover, Germany, 2Department of Gastroenterology and Hepatology, Hannover Medical School, Hannover, Germany, 3Department of Nephrology and Hypertension, Hannover Medical School, Hannover, Germany
Meeting: 2019 American Transplant Congress
Abstract number: 431
Keywords: Arteriosclerosis, Liver transplantation, Post-transplant hypertension, Risk factors
Session Information
Session Name: Concurrent Session: Liver Transplant Complications and Retransplantation II
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:30pm-2:42pm
Presentation Time: 2:30pm-2:42pm
Location: Ballroom A
*Purpose: Liver transplantation (LT) patients are prone to cardiovascular (CV) morbidity, since LT-related factors can add to the burden of classical risk factors. The aim of our study was to assess CV target organ damage and characterize associated risk factors in a prospective cohort study.
*Methods: We included 138 adult patients (age 52.3 ± 11.6 years) on the waiting list or after LT (5.4 ± 6.9 years post LT) and followed them over a period of 3.6 years. Annual assessments included measures of subclinical target organ damage such as pulse-wave velocity (PWV, a measure for arteriosclerosis), intima-media thickness (IMT, reflecting atherosclerosis) and left ventricular mass index (LVMI, for left ventricular hypertrophy), as well as CV risk factors.
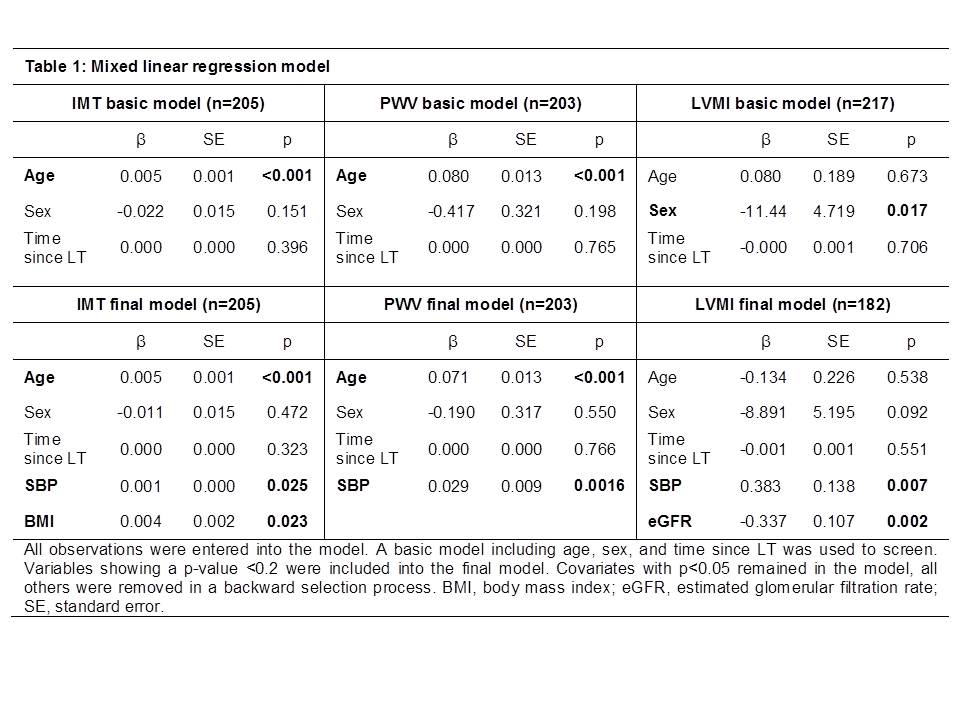
*Results: Prevalence of CV risk factors was high, with at least a quarter of patients suffering from metabolic syndrome, or displaying decreased renal function. A fifth of the patients showed at least one sign of subclinical target organ damage. Mixed linear regression modeling revealed higher systolic blood pressure (SBP), age and body-mass index to be independently associated with higher IMT; and higher age and SBP with higher PWV. Higher LVMI was associated higher SBP and lower estimated glomerular filtration rate (Table 1).
*Conclusions: Surprisingly LT-related factors (such as use of immunosuppressive drugs, or time since LT) were not independently associated with any of the outcome measures, suggesting that classical CV risk factors still remain the major culprits for CV disease. Our results show that CV disease burden is high after LT and that classical CV risk factors, especially blood pressure; should be a target of post-transplant care.
To cite this abstract in AMA style:
Kuepper C, Memaran N, Borchert B, Wick Avon, Bauer E, Jäckel E, Ziegert S, Schmidt BM, Melk A. Factors Associated with Cardiovascular Subclinical Target Organ Damage in Liver Transplant Recipients [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/factors-associated-with-cardiovascular-subclinical-target-organ-damage-in-liver-transplant-recipients/. Accessed February 27, 2026.« Back to 2019 American Transplant Congress