Pancreata From Donors With Renal Insufficiency: Viable For Transplant?
1Section of Abdominal Transplant Surgery, Washington University School of Medicine, St. Louis, MO, 2Department of Surgery, Johns Hopkins University, Baltimore, MD, 3Division of Nephrology, Washington University School of Medicine, St. Louis, MO
Meeting: 2019 American Transplant Congress
Abstract number: 403
Keywords: Allocation, Pancreas, Pancreas transplantation, Renal dysfunction
Session Information
Session Name: Concurrent Session: Pancreas and Islet: All Topics II
Session Type: Concurrent Session
Date: Monday, June 3, 2019
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:06pm-5:18pm
Presentation Time: 5:06pm-5:18pm
Location: Room 209
*Purpose: Pancreata are declined for transplantation for a multitude of reasons. Some of those reasons are organ edema as well as the potential for ischemic injury not able to be visualized at the time of procurement. The purpose of this abstract is to determine if the utilization of pancreata from donors with renal insufficiency is a safe practice.
*Methods: We identified 5,534 adult deceased donor pancreas-alone transplant (PTA) recipients between 2000 and 2018 from SRTR data. We further categorized the recipients into “discarded” group (pancreata from donors whose kidneys were discarded), “high creatinine” group (pancreata from donors whose kidneys were transplanted and who had a TC>1.5), and “low creatinine” group (pancreata from donors whose kidneys were transplanted with TC<1.5). We compared all-cause pancreas graft failure and mortality between the three groups. Cox regression was used to adjust for donor and recipient characteristics.
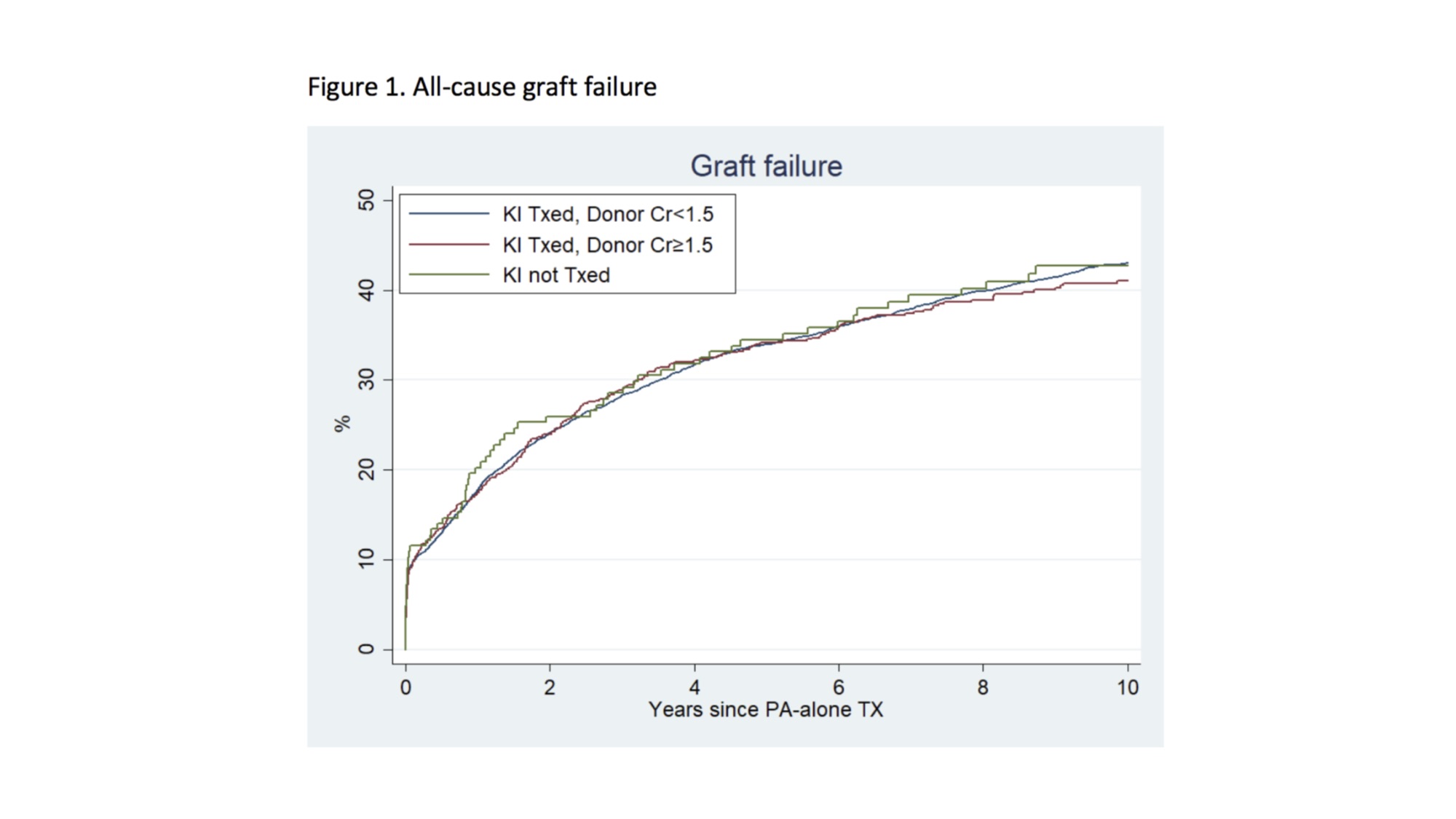
*Results: Among 5,534 pancreas recipients, 164 (3.0%) recipients had PTA from donors with discarded kidneys, and 664 (12.0%) recipients had PTA from high creatinine donors. At five years post-transplant, graft failure was 34.5%, 34.1%, and 34.0% for discarded, high creatinine, and low creatinine PTA recipients respectively (Figure 1). After adjustment, the discarded group (aHR: 0.821.051.32, p=0.7) and high creatinine group (aHR: 0.850.971.11, p=0.6) had similar risk of graft failure compared to low creatinine group (Table 1). Mortality at five years was 13.7%, 14.2% and 12.0% for discarded, high creatinine, and low creatinine, PTA recipients respectively (Figure 2). After adjustment, the discarded group had an 18% higher risk of mortality (aHR: 0.871.181.62, p=0.3) which is similar risk based on the CI, compared to low creatinine group. However, high creatinine had 29% higher risk of mortality (aHR: 1.091.291.53, p=0.003) than low creatinine group (Table 1).
*Conclusions: Donor renal insufficiency did not confer higher risk of pancreas graft failure among PTA recipients, but may confer higher risk of post-transplant mortality. In selected scenarios, pancreata from donors with renal insufficiency may be a safe mechanism to expand the donor pool.
To cite this abstract in AMA style:
Luo X, Wang JGaronzik, Doyle MB, Khan A, Alhamad T, Chapman WC, Massie A, Segev D, Wellen JR. Pancreata From Donors With Renal Insufficiency: Viable For Transplant? [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/pancreata-from-donors-with-renal-insufficiency-viable-for-transplant/. Accessed February 8, 2026.« Back to 2019 American Transplant Congress