Utilization of Donor Kidneys with Acute Kidney Injury in Pediatric Transplantation
1Surgery, UT Southwestern, Dallas, TX, 2Medicine, UT Southwestern, Dallas, TX
Meeting: 2019 American Transplant Congress
Abstract number: 131
Keywords: Donors, marginal, Kidney transplantation, Pediatric, Renal injury
Session Information
Session Name: Concurrent Session: Kidney: Pediatrics I
Session Type: Concurrent Session
Date: Sunday, June 2, 2019
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:30pm-4:42pm
Presentation Time: 4:30pm-4:42pm
Location: Room 304
*Purpose: Donor kidneys that are otherwise healthy with acute kidney injury (AKI) are increasingly used in adult transplant programs. We sought to examine the experience using kidneys with AKI in pediatric recipients.
*Methods: Outcomes from all pediatric kidney transplants between 1993 to 2018 documented in the Scientific Registry of Transplant Recipients (SRTR) database were collected. AKI was defined as a donor terminal creatinine of >2.0 mg/dL. Pediatric patients were defined as a recipients <18 years. Recipients of living donor kidneys and multi-organ transplants were excluded from the analysis. The pediatric patients were further divided by donor AKI status, era of transplantation (prior to 1990, 1990-1999, 2000-2009, and 2010-2018), high vs. low volume pediatric kidney transplant center (high volume being defined as a program that has performed > 100 kidney transplants in its history), and UNOS Regions. Donor and recipient demographic data were examined, and survival and outcomes were examined. A p-value of <0.05 was considered significant.
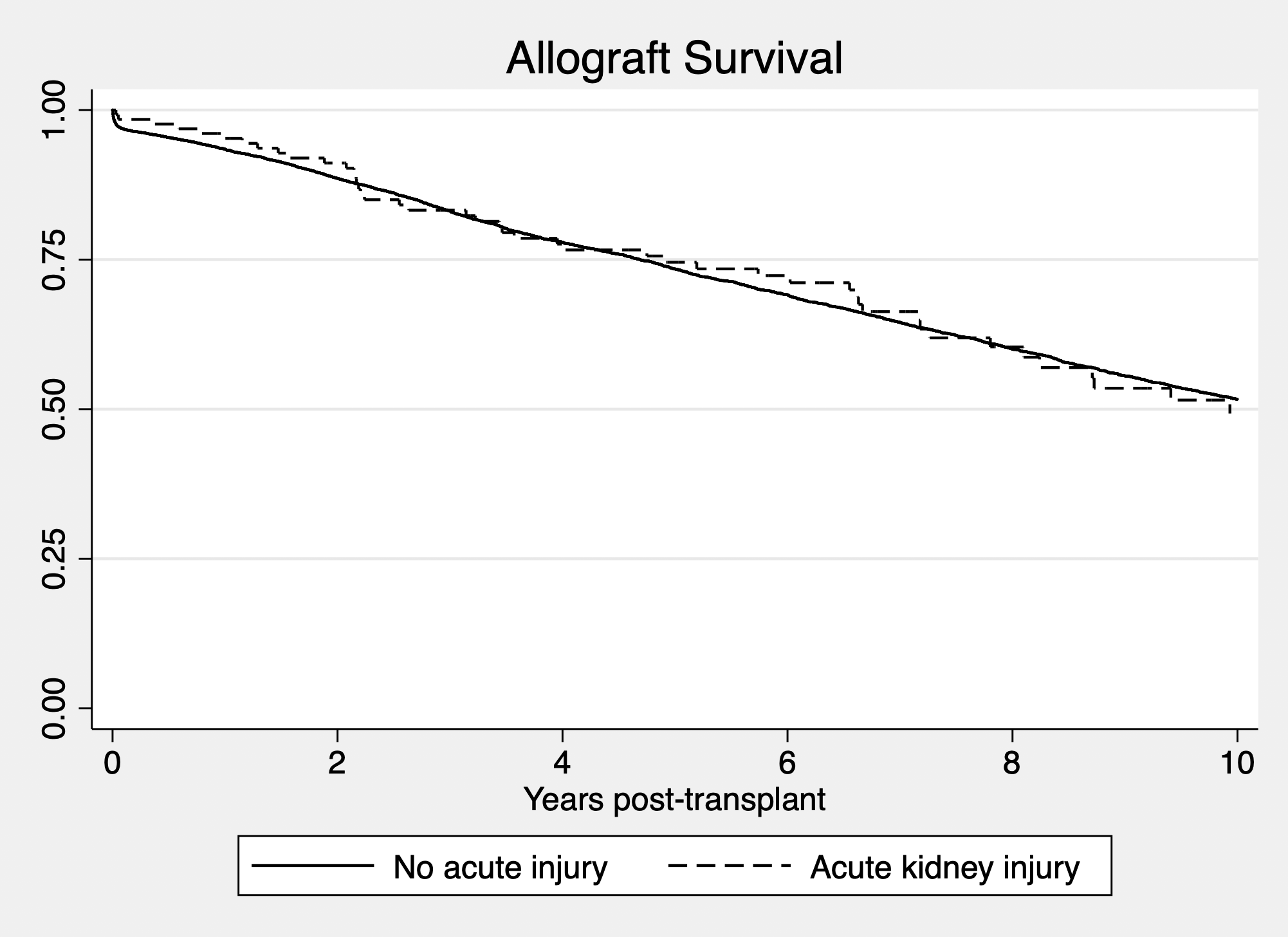
*Results: 9,900 pediatric kidney transplants were performed over this time period, of which 131 were AKI donors (1.3%). Based upon era, there was no difference in utilization rates. There was a significant difference in between use of these kidneys across regions, where Region 9 was the most likely to transplant an AKI kidney (3.3%) vs. Region 1 being the lowest utilizer (0.29%; p < 0.05). There were no significant differences between the share characteristics of the organ (local vs. regional vs. national; 80.1% vs. 10.7% vs. 9.1%; p = NS). There were also no significant differences between the HLA mismatch in the AKI vs. non AKI groups (4.3 vs. 4.4, p = NS), initial cPRA (5.7% vs. 2.9%, p = NS), end cPRA (12.4% vs 9.5%, p = NS), length of stay (9.8 vs. 11.2 days, p = NS). Serum Cr in the AKI group was significantly higher at time of discharge (1.97 vs. 1.41 mg/dL, p < 0.05). Allograft survival was not different between the groups. Interestingly, rates of delayed graft function (DGF) were not significantly different between the two groups (12.2% vs. 10.8%, p = NS, AKI vs. non AKI group).
*Conclusions: Outcomes of kidneys with AKI are comparable to those without AKI in the pediatric kidney transplant population. Despite a higher serum creatinine at the time of discharge, the recipients of AKI kidneys are not more likely to suffer from DGF. AKI kidneys are an untapped source of kidneys for the pediatric transplant recipients and should be strongly considered for use in this patient population.
To cite this abstract in AMA style:
Hwang CS, Tanriover B, Levea S, Desai D, Ariyamuthu V, Vagefi P, MacConmara M. Utilization of Donor Kidneys with Acute Kidney Injury in Pediatric Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/utilization-of-donor-kidneys-with-acute-kidney-injury-in-pediatric-transplantation/. Accessed February 11, 2026.« Back to 2019 American Transplant Congress