Shortened Cold Ischemia Time and Reduced Incidence of Delayed Graft Function for Kidney Transplants through Enhanced Tissue Compatibility Testing
1Transplantation and Liver Surgery, Helsinki University Hospital, Helsinki, Finland
2Histocompatibility Laboratory, Finnish Red Cross Blood Service, Helsinki, Finland.
Meeting: 2018 American Transplant Congress
Abstract number: D58
Keywords: Cadaveric organs, Histocompatibility, HLA matching
Session Information
Session Name: Poster Session D: Ischemia Reperfusion Injury: Time to Change the Fate?
Session Type: Poster Session
Date: Tuesday, June 5, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
A. HLA-typing and prospective leukocyte cross-matching needed for deceased donor kidney transplantation (kTX) may delay the onset of surgery. We compared cold ischemia times (CIT) before and after upgrading of histocompatibility tests. The effect of these changes to delayed graft function (DGF) and incidence of early rejections were assessed.
B. All recipients of a deceased donor kidney transplant in our center between 9.10.2013-16.10.2017 (N=896) were included. Traditional method of using density gradient-purified spleen cells for cross-matching was replaced on 12th of October 2015 with purification of peripheral blood T- and B-cells using RosetteSep®-kits (Stemcell Technologies). In addition, serology and SSP for donor HLA typing were replaced with LINKSEQ® qPCR method (Linkage Biosciences). Time consumed for laboratory tests was calculated from all suitable deceased donor studies performed in 2014 (n=101) and in 2016 (n=104). Altogether 442 patients receiving a transplant in the selected era of the old cross-match were compared with 454 patients with the new cross-match. DGF was defined as the need for post-transplant dialysis during the first week after transplantation.
C. Total time consumed for all histocompatibility tests decreased from mean 15h 7min to 8h 56min (p<0,001).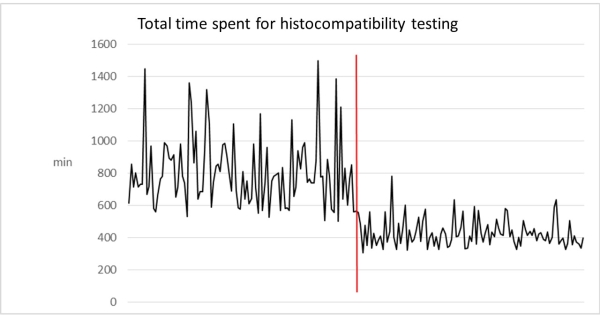 Reduction was greatest in cross-matches; from mean 8h 51min to 3 h 20min (p<0,001). CIT shortened from mean 20h 6min to 15h 52min (p<0,001). The incidence of DGF was significantly reduced from 31% to 24% (P=0.01). Among patients with DGF, the number of hemodialysis sessions did not differ, with median 3 sessions in both groups (range 1-30). The groups did not differ in the frequency of acute cellular (10% vs 13%) or antibody-mediated rejection (5% vs 3%).
Reduction was greatest in cross-matches; from mean 8h 51min to 3 h 20min (p<0,001). CIT shortened from mean 20h 6min to 15h 52min (p<0,001). The incidence of DGF was significantly reduced from 31% to 24% (P=0.01). Among patients with DGF, the number of hemodialysis sessions did not differ, with median 3 sessions in both groups (range 1-30). The groups did not differ in the frequency of acute cellular (10% vs 13%) or antibody-mediated rejection (5% vs 3%).
D. Optimization of histocompatibility tests help to reduce kTX cold ischemia time and the occurrence of DGF. Future development is warranted to optimize crosstalk between the tissue typing laboratory and transplant center to further minimize delays.
CITATION INFORMATION: Helanterä I., Saarinen T., Peräsaari J., Lempinen M., Lauronen J. Shortened Cold Ischemia Time and Reduced Incidence of Delayed Graft Function for Kidney Transplants through Enhanced Tissue Compatibility Testing Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Helanterä I, Saarinen T, Peräsaari J, Lempinen M, Lauronen J. Shortened Cold Ischemia Time and Reduced Incidence of Delayed Graft Function for Kidney Transplants through Enhanced Tissue Compatibility Testing [abstract]. https://atcmeetingabstracts.com/abstract/shortened-cold-ischemia-time-and-reduced-incidence-of-delayed-graft-function-for-kidney-transplants-through-enhanced-tissue-compatibility-testing/. Accessed March 6, 2026.« Back to 2018 American Transplant Congress
