Identifying Differences in Antimicrobial Resistance with a Liver Transplant Antibiogram
Methodist Dallas Medical Center, Dallas.
Meeting: 2018 American Transplant Congress
Abstract number: C329
Keywords: Bacterial infection, Infection, Liver transplantation
Session Information
Session Name: Poster Session C: Transplant Infectious Diseases
Session Type: Poster Session
Date: Monday, June 4, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Regulatory requirements for antimicrobial stewardship pose a unique challenge in special populations including transplant recipients. Infection following liver transplant can adversely impact patient outcomes. Moreover, orthotopic liver transplant (OLT) recipients are at an increased risk of infection with multidrug resistant organisms. In an effort to appropriately tailor empiric antimicrobial regimens, some have recommended generating transplant specific antibiograms. To better serve transplant patients, our institution created an OLT specific antibiogram (LTA) to improve antimicrobial stewardship.
A retrospective chart review of OLT patients at a single transplant center from January 2012 to October 2017 was performed. Only the first positive culture post-transplant was used. The LTA was compared to the 2016 hospital-wide antibiogram (HWA) using appropriate statistical tests.
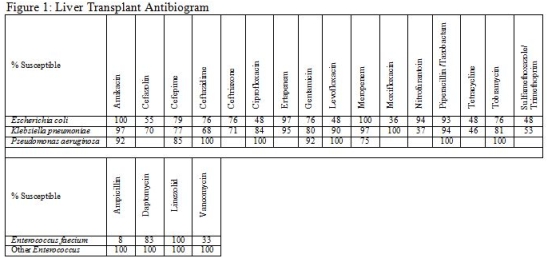
The LTA includes 87 of 325 patients transplanted during this time with 126 unique cultures. Of the positive cultures 32% were from blood, 57% from urine, and 10% from other sources. Figure 1 shows the susceptibility of key organisms to several antimicrobials.
There were several substantial differences noted between the LTA and HWA. ESBL producing E. coli (19 vs 11%; P=0.14) and Klebsiella spp. (23 vs 7.6%; P=0.012) were more commonly identified in OLT recipients. Pseudomonas isolates were less likely to be susceptible to meropenem (75 vs 92%; P=0.078), though the number of isolates was limited (n=12). Enterococci from OLT recipients were less likely to be susceptible to ampicillin (44 vs 77%; P<0.001) and vancomycin (59 vs 81%; P=0.004) driven by an increased prevalence of E. faecium (60 vs 26%; p<0.001).
The results highlighted increased infections with resistant organisms among transplant recipients. Creation of a transplant specific antibiogram allows providers to better tailor empiric therapy, monitor resistance rates and improve stewardship efforts in this unique patient population.
CITATION INFORMATION: Rago J., Crotty M., Milas E., Dominguez E. Identifying Differences in Antimicrobial Resistance with a Liver Transplant Antibiogram Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Rago J, Crotty M, Milas E, Dominguez E. Identifying Differences in Antimicrobial Resistance with a Liver Transplant Antibiogram [abstract]. https://atcmeetingabstracts.com/abstract/identifying-differences-in-antimicrobial-resistance-with-a-liver-transplant-antibiogram/. Accessed February 13, 2026.« Back to 2018 American Transplant Congress