Multi-Visceral Transplant in an HIV Positive Recipient – One Year Survival
S. Nagaraju, R. Mangus, J. Fridell.
Surgery, Indiana University School of Medicine, Indianapolis, IN.
Meeting: 2018 American Transplant Congress
Abstract number: C306
Keywords: Epstein-Barr virus (EBV), HIV virus, Multivisceral transplantation, Post-transplant lymphoproliferative disorder (PTLD)
Session Information
Session Name: Poster Session C: Small Bowel: All Topics
Session Type: Poster Session
Date: Monday, June 4, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Human immunodeficiency virus (HIV) is associated with hypercoagulability and thrombotic events. Highly active anti-retroviral therapy (HAART) has improved long term survival. More patients with HIV are undergoing solid organ transplantation. Multi-visceral transplant (MVT) is offered to patients with intestinal failure and liver disease. Until now there has been one case report of an en-bloc MVT with kidney transplantation in a HIV positive recipient with only 3 month survival of patient. We here report the longest survival of (425 days) a HIV positive recipient who underwent a MVT for diffuse porto-mesenteric thrombosis, short-gut syndrome and liver fibrosis.
Patient was a 53 year old Caucasian female with HIV (type 1) without AIDS/AIDS defining illnesses, maintained on HAART regimen for 10 years and porto-mesenteric thrombosis with liver fibrosis. She developed acute bowel perforation, needing a laparotomy with small bowel resection resulting in short gut syndrome. She had an undetectable viral load, CD4 count 184 cells/mm3 and positive Eppstein-Barr virus (EBV) IgG prior to transplant. She was on HAART regime of oral emtricitabine and tenofovir. She underwent MVT with arterial inflow from the infra renal aorta and venous outflow though native hepatic veins. Induction immunosuppression was with steroids, antithymocyte globulin (4.5mg/kg), and rituximab (150mg/m2). Maintenance immunosuppression consisted of tacrolimus (goal trough level 10-15 ng/mL) and low dose oral prednisone. Raltegravir was added to HAART. She was discharged home on oral diet on POD 110.
She was readmitted for bowel perforation and a liver mass, 8 months after transplant. She underwent resection of hepatic mass and intestine segments which stained positive for EBV, lowering of immunosuppression, rituximab therapy initially, followed by 3 cycles of chemotherapy with Rituximab, Cyclophosphamide, Doxorubicin, Vincristine and prednisolone. Patient subsequently developed bone marrow suppression, pancytopenia and sepsis which ultimately led to her death on post-operative day 425. 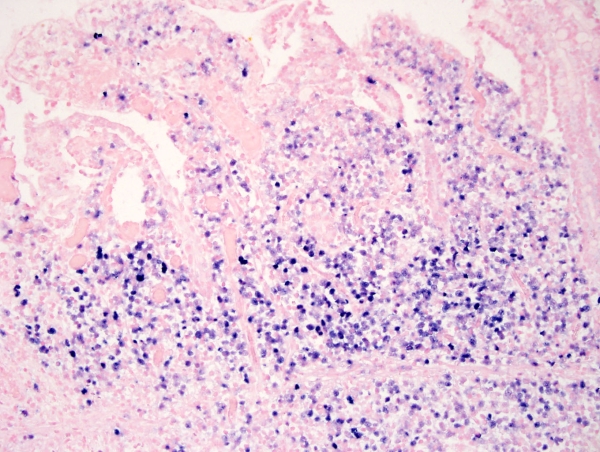 Conclusion:Successful intestinal transplant can be achieved in HIV positive individuals.
Conclusion:Successful intestinal transplant can be achieved in HIV positive individuals.
CITATION INFORMATION: Nagaraju S., Mangus R., Fridell J. Multi-Visceral Transplant in an HIV Positive Recipient – One Year Survival Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Nagaraju S, Mangus R, Fridell J. Multi-Visceral Transplant in an HIV Positive Recipient – One Year Survival [abstract]. https://atcmeetingabstracts.com/abstract/multi-visceral-transplant-in-an-hiv-positive-recipient-one-year-survival/. Accessed January 5, 2026.« Back to 2018 American Transplant Congress
