National Outcomes of Donor and Recipient Sex Mismatch in Kidney Transplantation
1Transplant Surgery, Tampa General Medical Group, Tampa General Hospital, Tampa, FL
2Transplant Research, Tampa General Hospital, Tampa, FL
3Molecular Pharmacology & Physiology, University of South Florida, Tampa, FL.
Meeting: 2018 American Transplant Congress
Abstract number: C57
Keywords: Graft survival, Kidney transplantation, Outcome
Session Information
Session Name: Poster Session C: Kidney Donor Selection / Management Issues
Session Type: Poster Session
Date: Monday, June 4, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Introduction: Gender Outcomes remain controversial in solid organ transplantation.
Aim: The study aim was to evaluate the outcomes of sex mismatched donors and recipients where a single donor was transplanted in both a male and female recipient.
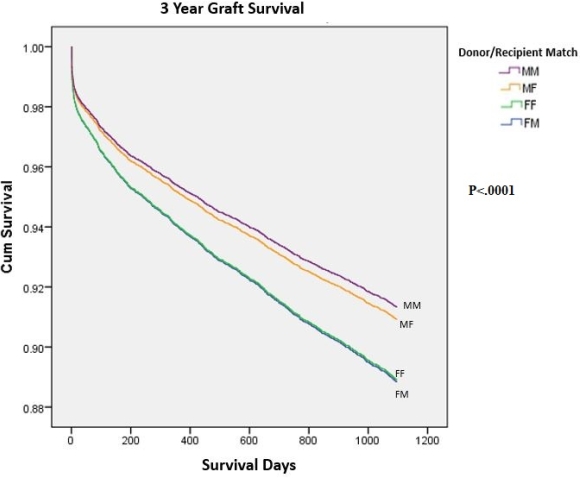
Methods: Using OPTN data, we conducted a retrospective cohort study of kidney transplants (KT) from January 2006 through December 2013. We grouped data based on four categories: 1) Male donor to male recipient (MM), 2) Male donor to female recipient (MF), 3) Female donor to female recipient (FF), and 4) Female donor to male recipient (FM). Time to event data were analyzed using cox-regression and summarized as hazard ratio (HR) along with 95% confidence interval (CI).
Results: Nationally, there were 140,842 kidney transplants performed. We excluded donors with same sex recipients, pediatric patients, living donors, bilateral/en-bloc recipients, multi-organ recipients, and preemptive transplants which left 8,057 pairs of two-sex adult recipients from single adult deceased donors (N=16,114). There were no differences between groups based on length of stay (P=.263), cold ischemic time (P=.454), and 3-year patient survival (P=.234). However, discharge creatinine was significant MM (4.18), MF (3.03), FF (3.12), and FM (4.13); P<.0001. Delayed graft function was significant for MM (33.5%) when compared to MF (25.9%), FF (24.6%), and FM (30.1%); P<.0001. The difference in three year graft survival was statistically significant favoring MM compared with FF (HR=1.30; 95% CI 1.13 to 1.50; P<.0001) and MM compared with FM (HR=1.31; 95% CI 1.13 to 1.50; P<.0001).
Conclusion: The national use of sex mismatched donors and recipients for deceased donor kidney transplantation resulted in statistically significant lower 3-year graft survival for female donors to male recipients. Although the use of sex mismatched donors and recipients may be unavoidable, these outcomes should be considered when attempting to optimize the best graft survival for recipients.
CITATION INFORMATION: Buggs J., Wang L., Liu R., Rogers E., Bowers V. National Outcomes of Donor and Recipient Sex Mismatch in Kidney Transplantation Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Buggs J, Wang L, Liu R, Rogers E, Bowers V. National Outcomes of Donor and Recipient Sex Mismatch in Kidney Transplantation [abstract]. https://atcmeetingabstracts.com/abstract/national-outcomes-of-donor-and-recipient-sex-mismatch-in-kidney-transplantation/. Accessed February 22, 2026.« Back to 2018 American Transplant Congress