Correlation of Kidney Transplant Human Leukocyte Antigen Eplet Mismatching to De Novo Donor Specific Antibody Production and Post-Transplant Outcomes
1Department of Pharmacy, Universitty of North Carolina Medical Center, Chapel Hill, NC
2Department of Surgery, Universitty of North Carolina Medical Center, Chapel Hill, NC
3Department of Pharmacy, Ochsner Health System, New Orleans, LA
4Department of Pathology, University of North Carolina Medical Center, Chapel Hill, NC.
Meeting: 2018 American Transplant Congress
Abstract number: C8
Keywords: Antibodies, Epitopes, Histocompatibility antigens, HLA matching
Session Information
Session Name: Poster Session C: Histocompatibility and Immunogenetics
Session Type: Poster Session
Date: Monday, June 4, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Human Leukocyte Antigen (HLA) eplet mismatches (EMM) are associated with the development of de novo donor specific antibody (dnDSA) in kidney transplant recipients (KTRs). There is limited data assessing the impact of EMM on dnDSA in highly sensitized KTRs or with alemtuzumab induction (ATZi). The aim of this study was to correlate EMM with dnDSA incidence, acute rejection (AR), patient and graft survival in KTRs receiving ATZi.
A single center retrospective analysis of 318 adult KTRs was performed from January 1, 2013 – December 31, 2016. KTRs with prior non-kidney or dual organ transplant (TXP), ABO incompatible TXP, or non-ATZi were excluded. HLAMatchmaker was used to enumerate EMM. KTRs were stratified based on dnDSA development (single antigen bead MFI ≥ 1000) at 6 months (mo) and further categorized by the number of EMM: 0-5, 6-10, and >10. Incidence of dnDSA within 6 mo and AR within 12 mo were analyzed. Chi-squared test for categorical variables and T-test for continuous variables were performed (p < 0.05 = significance). Three-year graft and patient survival rates were analyzed using Kaplan-Meier estimates.
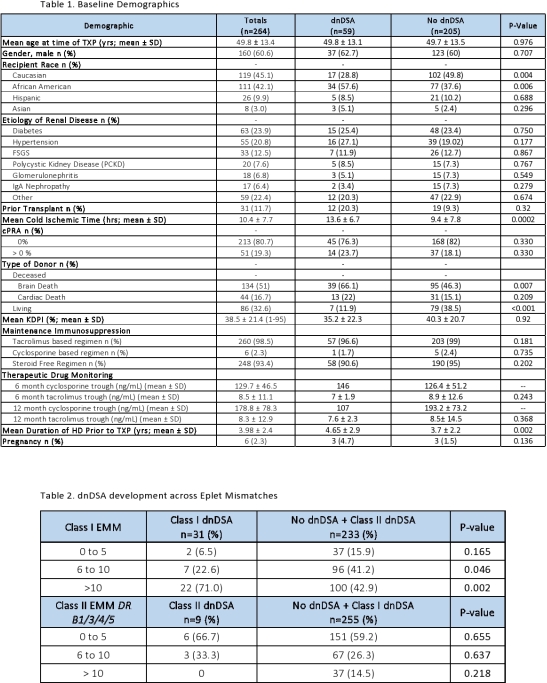
264 KTRs met inclusion criteria. 59 (22%) KTRs developed dnDSA at 6 mo v. 205 (78%) did not. Baseline TXP characteristics are described in Table 1. Of those that developed dnDSA, 31 (53%) KTRs had class I dnDSAs v. 28 (47%) had class II dnDSAs. Incidence of AR, graft and patient survival were similar between groups. Class I dnDSA was significantly higher in EMM ≥ 6; however, no difference was seen in DR dnDSA across EMM (Table 2). DQ dnDSA data is pending.
EMM ≥ 6 was significantly associated with class I dnDSA 6 mo post-TXP in KTRs who received ATZi.
CITATION INFORMATION: Samudralwar R., Szempruch K., Reuter C., Franz B., Lee R., Weimer E., Detwiler R., Kozlowski T., Schmitz J. Correlation of Kidney Transplant Human Leukocyte Antigen Eplet Mismatching to De Novo Donor Specific Antibody Production and Post-Transplant Outcomes Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Samudralwar R, Szempruch K, Reuter C, Franz B, Lee R, Weimer E, Detwiler R, Kozlowski T, Schmitz J. Correlation of Kidney Transplant Human Leukocyte Antigen Eplet Mismatching to De Novo Donor Specific Antibody Production and Post-Transplant Outcomes [abstract]. https://atcmeetingabstracts.com/abstract/correlation-of-kidney-transplant-human-leukocyte-antigen-eplet-mismatching-to-de-novo-donor-specific-antibody-production-and-post-transplant-outcomes/. Accessed February 20, 2026.« Back to 2018 American Transplant Congress