Impact of Immunogenicity on Kidney Allograft Survival in Patients Treated with Induction Therapy
University of Toledo, Toledo.
Meeting: 2018 American Transplant Congress
Abstract number: B127
Keywords: Immunogenicity, Kidney transplantation, Survival
Session Information
Session Name: Poster Session B: Kidney Immunosuppression: Induction Therapy
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Background. The induction therapy is currently used in the majority of kidney transplant recipients, regardless of their level of donor/recipient compatibility. We examined whether lower immunogenicity (IM) between donor and recipient improved allograft survivals in groups of recipients treated with three different induction therapies or without induction.
MethodsResults. We analyzed 30,648 deceased kidney transplants from 2009 to 2011 (SRTR database): 25,528 were with induction, namely 14,675 with anti-thymocyte globulin (equine or rabbit, ATG), 4,139 with anti-CD52 mAb (alemtuzumab, Alem), 6,714 with interleukin-2 receptor inhibitor (basiliximab, IL2-RI), whereas 5,120 remained without any induction. HLA-A/B/DR of donors and recipients were imputed from 2-digit to 4-digit HLAs by HaploStats algorithm. Each donor/recipient pair's immunogenicity (IM) was then estimated by the Kosmoliaptsis algorithm, namely electrostatic mismatch score (EMS); pairs with IM scores above median (50th percentile) were considered as high EMS IM and below as low EMS IM. The 5-year death-censored graft survival for all induction groups combined was better than without induction (p <0.001; Fig. 1A 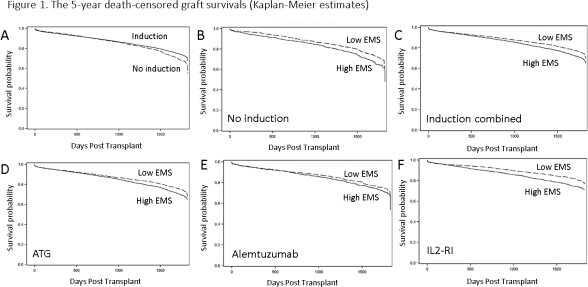 ); each of three induction groups (ATG, Alem, IL2-RI) was also superior to no induction (p <0.001; not shown). When no induction group (Fig. 1B), all induction groups combined (Fig. 1C), and each of the induction groups (ATG, Fig. 1D; Alem, Fig. 1E; and IL2-RI, Fig. 1F) were stratified by IM (EMS), there was a significant difference in the survival between low and high EMS groups (p <0.05; except of Alem, p=0.14). High and low IM groups for each induction therapy had the same distribution of HLA-A/B/DR mismatches: i.e. more pairs with 0-3 mismatches and less pairs with 5/6 mismatches in low IM groups vs. less pairs with 0-3 mismatches and more with 5/6 mismatches in high IM groups.
); each of three induction groups (ATG, Alem, IL2-RI) was also superior to no induction (p <0.001; not shown). When no induction group (Fig. 1B), all induction groups combined (Fig. 1C), and each of the induction groups (ATG, Fig. 1D; Alem, Fig. 1E; and IL2-RI, Fig. 1F) were stratified by IM (EMS), there was a significant difference in the survival between low and high EMS groups (p <0.05; except of Alem, p=0.14). High and low IM groups for each induction therapy had the same distribution of HLA-A/B/DR mismatches: i.e. more pairs with 0-3 mismatches and less pairs with 5/6 mismatches in low IM groups vs. less pairs with 0-3 mismatches and more with 5/6 mismatches in high IM groups.
Conclusions: 1) Independently of the induction protocol low EMS IM donor/recipient pairs display better graft survival than high EMS IM pairs; 2) Selection of low IM donor/recipient pairs by EMS may improve long-term kidney allograft survivals; and 3) 5/6 HLA mismatches have low IM pairs.
CITATION INFORMATION: Bekbolsynov D., Mierzejewska B., Rees M., Ortiz J., Ekwenna O., Stepkowski S. Impact of Immunogenicity on Kidney Allograft Survival in Patients Treated with Induction Therapy Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Bekbolsynov D, Mierzejewska B, Rees M, Ortiz J, Ekwenna O, Stepkowski S. Impact of Immunogenicity on Kidney Allograft Survival in Patients Treated with Induction Therapy [abstract]. https://atcmeetingabstracts.com/abstract/impact-of-immunogenicity-on-kidney-allograft-survival-in-patients-treated-with-induction-therapy/. Accessed February 25, 2026.« Back to 2018 American Transplant Congress
