Racial Disparities in Post-Liver Transplant Survival before and after Share 35 Implementation
1Department of Epidemiology, Rollins School of Public Health, Atlanta, GA
2Emory Transplant Center, Atlanta, GA.
Meeting: 2018 American Transplant Congress
Abstract number: A304
Keywords: African-American, Liver transplantation, Outcome, Survival
Session Information
Session Name: Poster Session A: Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Type: Poster Session
Date: Saturday, June 2, 2018
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall 4EF
Background: The Share 35 policy was intended to improve equity in access to liver transplantation by broadening regional sharing of livers for the sickest patients (listed with a MELD score > 35). Recent studies have found one-year survival for patients with a MELD > 35 improved after the implementation of Share 35 in June 2013. We used data from the Scientific Registry of Transplant Recipients (SRTR) to assess if racial disparities in post-transplant survival improved in the Share 35 era.
Methods: Patients were included if they were white or black and received a liver transplant in the U.S. between June 18th, 2011 and June 17th, 2015 (2 years pre- and post- Share 35 implementation). The primary outcome was 1-year patient survival after transplant. Black-white hazard ratios were calculated using Cox regression and adjusted for age, gender, MELD, underlying cause of disease, distance from the transplant center, community socioeconomic status (SES), donor risk status and UNOS region. In addition, we conducted stratified analyses by MELD to determine if disparities were consistent across MELD categories.
Results: Our analysis included 22,936 liver recipients; approximately 11% were black. There was significant interaction between race and Share 35 era (p = 0.03, 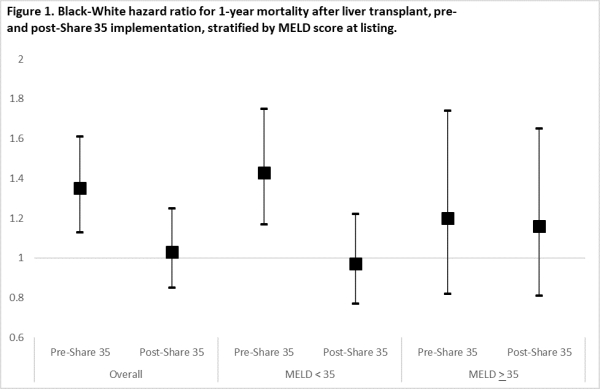 ). Prior to Share 35, black patients had a 35% excess risk of mortality in the first year after transplant (95% CI: 1.13, 1.61). After Share 35, there were no racial differences in 1-year survival. Among patients listed with MELD > 35, Share 35 had no effect on racial differences in post-transplant survival (p=0.90); interaction was only present among patients listed with a MELD < 35 (p=0.01).
). Prior to Share 35, black patients had a 35% excess risk of mortality in the first year after transplant (95% CI: 1.13, 1.61). After Share 35, there were no racial differences in 1-year survival. Among patients listed with MELD > 35, Share 35 had no effect on racial differences in post-transplant survival (p=0.90); interaction was only present among patients listed with a MELD < 35 (p=0.01).
Discussion: Racial disparities in post-transplant survival were reduced after Share 35 implementation. This effect was limited to patients listed with a MELD below 35, who were not the target of Share 35; observed reductions may not be attributable to changes in organ allocation policy. Further research is needed to elucidate the etiology of racial disparities in post-transplant outcomes and improve clinical care for vulnerable patients.
CITATION INFORMATION: Ross K., Lynch R., Patzer R. Racial Disparities in Post-Liver Transplant Survival before and after Share 35 Implementation Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Ross K, Lynch R, Patzer R. Racial Disparities in Post-Liver Transplant Survival before and after Share 35 Implementation [abstract]. https://atcmeetingabstracts.com/abstract/racial-disparities-in-post-liver-transplant-survival-before-and-after-share-35-implementation/. Accessed February 14, 2026.« Back to 2018 American Transplant Congress
