Interleukin-17 Deficiency Attenuates Renal Allograft Injury and Prolongs Survival in a Murine Transplantation Model
1Sydney Medical School, University of Sydney, Sydney, New South Wales, Australia
2Renal Medicine, Royal Prince Alfred Hospital, Sydney, New South Wales, Australia
3Discipline of Pathology, School of Medical Sciences, Sydney, New South Wales, Australia
4Centre for Kidney Research, The Children's Hospital at Westmead, Sydney, New South Wales, Australia.
Meeting: 2015 American Transplant Congress
Abstract number: D74
Keywords: Kidney transplantation, knockout, Mice, Rejection
Session Information
Session Name: Poster Session D: Innate Immunity in Transplantation
Session Type: Poster Session
Date: Tuesday, May 5, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Aim:
To investigate the role of IL-17 in allograft rejection using a murine model of fully MHC-mismatched renal transplantation.
Methods:
Life-sustaining kidney transplants were performed in nephrectomized mice: WT BALB/c to WT C57BL/6 (WT allografts), IL-17-/- BALB/c to IL-17-/- C57BL/6 (IL-17-/- allografts) and WT C57BL/6 to WT C57BL/6 (isografts). Mice were also sacrificed on days 14 and 100 post-transplantation for assessment of the acute and chronic rejection responses.
Results:
IL-17-/- allograft recipients had significantly improved survival as compared to WT allograft recipients (median survival >100 vs 37.5 days, p=0.031). Similar prolongation was achieved in WT allografts which received a neutralizing IL-17 antibody (median survival >100 days, p=0.027).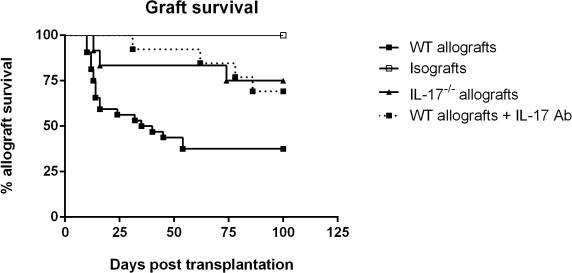 IL-17-/- allografts were protected against acute rejection with lower serum creatinine (26.22±1.75 vs 50.00±4.42μmol/L, p=0.0018) and less tubulitis (score 109.6±7.66 vs 158.3±9.65, p=0.0007) compared to WT allografts and isolated T cells produced less IFN-γ in response to ex vivo allostimulation (p<0.0001). By day 100, IL-17-/- allografts exhibited superior renal function (20.00±3.01 vs 48.75±9.48μmol/L, p=0.025), less proteinuria (0.41±0.20 vs 1.13±0.10mg/16hrs, p=0.0095) and reduced interstitial collagen deposition (13.48±2.49 vs 30.37±4.09% points positive, p=0.0082) compared to WT allografts. Subsequent experiments using either donors or recipients deficient in IL-17 showed a trend towards prolongation of survival only when the recipients were IL-17-/-. The survival advantage conferred by IL-17 deficiency was attenuated by depletion of CD4+CD25+ cells.
IL-17-/- allografts were protected against acute rejection with lower serum creatinine (26.22±1.75 vs 50.00±4.42μmol/L, p=0.0018) and less tubulitis (score 109.6±7.66 vs 158.3±9.65, p=0.0007) compared to WT allografts and isolated T cells produced less IFN-γ in response to ex vivo allostimulation (p<0.0001). By day 100, IL-17-/- allografts exhibited superior renal function (20.00±3.01 vs 48.75±9.48μmol/L, p=0.025), less proteinuria (0.41±0.20 vs 1.13±0.10mg/16hrs, p=0.0095) and reduced interstitial collagen deposition (13.48±2.49 vs 30.37±4.09% points positive, p=0.0082) compared to WT allografts. Subsequent experiments using either donors or recipients deficient in IL-17 showed a trend towards prolongation of survival only when the recipients were IL-17-/-. The survival advantage conferred by IL-17 deficiency was attenuated by depletion of CD4+CD25+ cells.
Conclusion:
Renal allograft rejection was attenuated, survival prolonged and long term graft function improved in the absence of IL-17. This is likely due to impaired development of Th1 alloimmunity and is CD4+CD25+ dependent.
To cite this abstract in AMA style:
Kwan T, Chadban S, Ma J, Bao S, Alexander S, Wu H. Interleukin-17 Deficiency Attenuates Renal Allograft Injury and Prolongs Survival in a Murine Transplantation Model [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/interleukin-17-deficiency-attenuates-renal-allograft-injury-and-prolongs-survival-in-a-murine-transplantation-model/. Accessed January 7, 2026.« Back to 2015 American Transplant Congress
