Evaluating Center Performance beyond Patient and Graft Survival
Baylor University Medical Center, Dallas, TX.
Meeting: 2018 American Transplant Congress
Abstract number: 478
Keywords: Allocation, Liver transplantation, Morbidity, Public policy
Session Information
Session Name: Concurrent Session: Non-Organ Specific: Economics, Public Policy, Allocation, Ethics - 2
Session Type: Concurrent Session
Date: Tuesday, June 5, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:30pm-3:42pm
Presentation Time: 3:30pm-3:42pm
Location: Room 4C-4
Introduction: LT centers are judged by patient survival at 1-yr post LT; however risk incurred on the waitlist or center specific practices post LT are not captured. Alternate measures of morbidity and mortality before and after LT may more accurately capture center performance.
Methods: We examined all centers (blinded to center ID) performing LT using national data. Intent to treat (ITT) survival was patient death w/n 1 year from listing stratified by MELD score. Patient survival was from time of LT. Morbidity w/n 1 year after LT was: (a) initial LOS (b) multiple readmission (c) new CKD (Cr >2.5mg/dL, HD beyond 3mo, listing for KT), (d) new DM (e) HCC recurrence (f) poor functional status (g) employment status. Mixed effects/ frailty models were used to assess center variation.
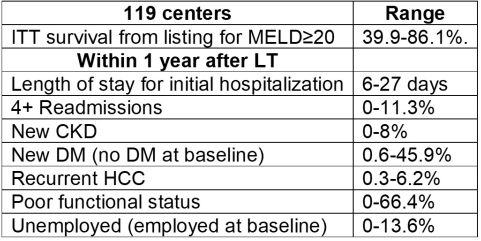
Results: Between 2002-15, there were 64,019 LT at 119 centers. Center variation in ITT survival by center for MELD score ≥ 20 (40-86%) was larger than 1 year survival after LT.(Figure 1a) There was wide variation in morbidity across centers.(Table) Even when limited to “top performing centers” (n=30) absolute 1 year pt survival varied by 8% (88-96%), but ITT survival for MELD ≥20 varied by 40% (47-86%).(Figure 1b) Morbidity after LT was variable: median LOS (7-27 days), 4 +readmissions (0-6%), CKD rates (0.2-8%), new DM (1-46%), HCC recurrence (0.5-4%), poor functional status (1.2-55%), and unemployment (1-9%). There was no correlation (r≤0.3, p=NS) between survival at a center and measures of morbidity. Correlation was r<0.5 stratified by MELD at LT and center volume except between highest center volume and LOS (r=0.6, p<0.01) and CKD (r=0.65, p<0.01).
Conclusion: Assessing ITT survival from listing and patient centered measures post LT may highlight differences in program quality and help adjudicate center performance beyond patient survival after LT.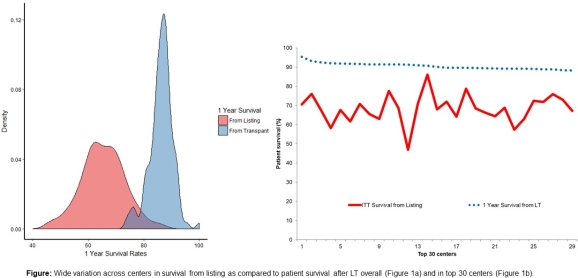
CITATION INFORMATION: Asrani S., Saracino G., Bahirwani R., McKenna G., Klintmalm G., Trotter J. Evaluating Center Performance beyond Patient and Graft Survival Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Asrani S, Saracino G, Bahirwani R, McKenna G, Klintmalm G, Trotter J. Evaluating Center Performance beyond Patient and Graft Survival [abstract]. https://atcmeetingabstracts.com/abstract/evaluating-center-performance-beyond-patient-and-graft-survival/. Accessed December 16, 2025.« Back to 2018 American Transplant Congress
