Pro-Inflammatory B Cells Predict Progressive Minimal Early Renal Allograft Inflammation Which is Associated with Poor Graft Outcomes
UPMC, Pittsburgh.
Meeting: 2018 American Transplant Congress
Abstract number: 408
Keywords: Inflammation, Rejection
Session Information
Session Name: Concurrent Session: Biomarkers, Immune Monitoring and Outcomes: Basic
Session Type: Concurrent Session
Date: Tuesday, June 5, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:30pm-3:42pm
Presentation Time: 3:30pm-3:42pm
Location: Room 602/603/604
The clinical significance of minimal tubulointerstitial inflammation (MTI:'t'+'i'scores 0.5-1.5) and Banff Borderline changes (BBC:'t'+'i'scores 2-3) in early renal allograft biopsies is unclear. The rate and significance of progression of these lesions to late acute rejection (AR) also remains unknown. Our center performs 2 protocol Bxs (3&12mo) along with for-cause Bxs. This allows us to assess the clinical impact of early(0-4mo)MTI and BBC on graft outcomes. 208/372 patients had either no inflammation(NI, 36%), MTI(34%) or BBC(30%) on early Bxs(0-4mo). Patients with NI(17%), MTI(24%) and BBC(34%) at 3mo exhibited increasing rates (in parentheses) of progression to AR (≥Banff 1A) by 12mo. Further, patients with MTI or BBC(3mo) had increased graft loss or impending graft loss (eGFR<30ml/min+ >30% fall from baseline) by 50mo when compared to those with NI(Fig 1A).While graft outcome in the NI group was not affected by progression to late AR(p=0.85), patients with early MTI(Fig 1B) or BBC(Fig 1C) had significantly worse outcomes if they developed late AR. Thus, early allograft inflammation (MIT or BBC) was not only associated with increased progression to late AR, but those who progressed had worse outcomes. Thus, MTI and BBC, particularly in patients who will progress, are a cohort with poor outcomes. However, clinical factors, including 3mo histology, could not predict progression. Based on previous results, we asked whether peripheral blood B cell cytokines could predict progression to AR. 72 patients with either MTI(n=26) or BBC(n=46) had their B cells analyzed at 3mos. IL10:TNFα expression ratio within T1 transitional B cells was significantly lower in both the MTI(6.3X↓) and BBC(4.6X↓) patients who progressed vs. stable (p<0.0004). Finally,a low T1B cytokine ratio strongly predicted late progression to AR (ROC AUC 0.94 p<0.0001 Sen 92% Spec 88%) in patients with early allograft inflammation(MIT or BBC). Thus, patients with early minimal allograft inflammation that progress to AR at 1yr represent a high-risk cohort for graft dysfunction. This group could be identified by 2-4 mo, using the T1B IL10:TNFα ratio–allowing early intervention.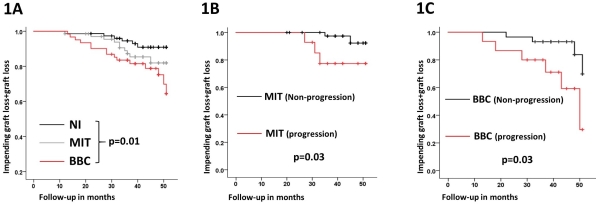
CITATION INFORMATION: Sharma A., Cherukuri A., Chittka D., Mehta R., Hariharan S., Rothstein D. Pro-Inflammatory B Cells Predict Progressive Minimal Early Renal Allograft Inflammation Which is Associated with Poor Graft Outcomes Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Sharma A, Cherukuri A, Chittka D, Mehta R, Hariharan S, Rothstein D. Pro-Inflammatory B Cells Predict Progressive Minimal Early Renal Allograft Inflammation Which is Associated with Poor Graft Outcomes [abstract]. https://atcmeetingabstracts.com/abstract/pro-inflammatory-b-cells-predict-progressive-minimal-early-renal-allograft-inflammation-which-is-associated-with-poor-graft-outcomes/. Accessed January 29, 2026.« Back to 2018 American Transplant Congress
