Increase in Potentially Resistant Non-Aspergillus Molds Isolated in Lung Transplant Recipients after Voriconazole and Posaconazole Prophylaxis
1Infectious Diseases, University of California San Francisco, San Francisco, CA
2Pulmonary and Critical Care, University of California San Francisco, San Francisco, CA.
Meeting: 2018 American Transplant Congress
Abstract number: 78
Keywords: Fungal infection, Infection, Lung transplantation, Prophylaxis
Session Information
Session Name: Concurrent Session: Lung: From Allocation to Outcomes
Session Type: Concurrent Session
Date: Sunday, June 3, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:06pm-3:18pm
Presentation Time: 3:06pm-3:18pm
Location: Room 303
Background: Lung transplant recipients are at higher risk for invasive fungal infections compared to other solid organs transplant patients. Antifungal prophylaxis with mold-active azoles has become common in this population, but few studies have examined its impact on the emergence of resistant fungal pathogens. We hypothesized that voriconazole and posaconazole prophylaxis would be associated with increased rates of potentially resistant non-Aspergillus molds.
Methods: We conducted a retrospective review of post-transplant bronchoalveolar lavage (BAL) culture results at our institution. We describe the non-Aspergillus molds isolated over time, and used Chi-squared tests to compare their prevalence before and after institution of voriconazole and posaconazole prophylaxis. We assessed risk factors for growth of non-Aspergillus molds using multivariate logistical regression.
Results: From 8/2000 to 2/2017, 557 subjects underwent BAL sampling, of whom 219 had 568 mold isolates cultured during 435 BAL events. The prevalence of non-Aspergillus molds has increased over time. 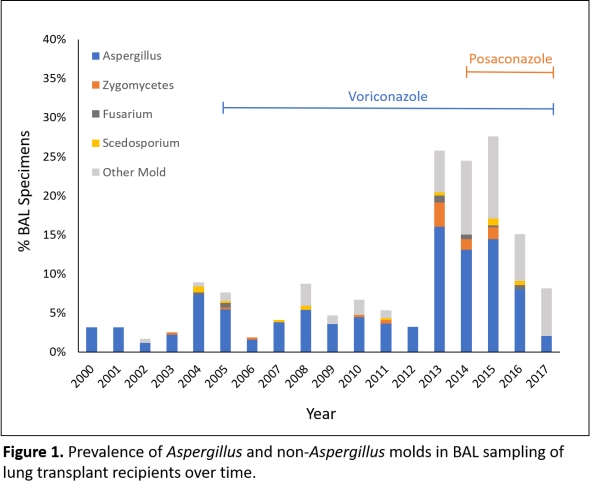 Common species include Penicillium, Rhizopus, Sporotrichum, Scedosporium, and Fusarium. Non-Aspergillus species were isolated in 0.9% of BAL specimens before versus 5.1% after (p<0.0001) standard voriconazole prophylaxis in 2005, and 2.5% before versus 9.8% after (p<0.0001) incorporating posaconazole prophylaxis in 2014. After adjusting for age, sex, indication for and time from transplant, antifungal prophylaxis with voriconazole (OR 2.60, 95%CI 1.14-5.93) and posaconazole (OR 4.71, 95%CI 2.07-10.74) was associated with isolation of non-Aspergillus molds.
Common species include Penicillium, Rhizopus, Sporotrichum, Scedosporium, and Fusarium. Non-Aspergillus species were isolated in 0.9% of BAL specimens before versus 5.1% after (p<0.0001) standard voriconazole prophylaxis in 2005, and 2.5% before versus 9.8% after (p<0.0001) incorporating posaconazole prophylaxis in 2014. After adjusting for age, sex, indication for and time from transplant, antifungal prophylaxis with voriconazole (OR 2.60, 95%CI 1.14-5.93) and posaconazole (OR 4.71, 95%CI 2.07-10.74) was associated with isolation of non-Aspergillus molds.
Conclusion: The prevalence of non-Aspergillus molds in lung transplants recipients appears to be increasing in association with voriconazole and posaconazole prophylaxis. This shift in microbiology to more potentially resistant molds may make treatment of invasive fungal disease more challenging in this immunocompromised population.
CITATION INFORMATION: Fung M., Greenland J., Hays S., Singer J., Golden J., Chin-Hong P. Increase in Potentially Resistant Non-Aspergillus Molds Isolated in Lung Transplant Recipients after Voriconazole and Posaconazole Prophylaxis Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Fung M, Greenland J, Hays S, Singer J, Golden J, Chin-Hong P. Increase in Potentially Resistant Non-Aspergillus Molds Isolated in Lung Transplant Recipients after Voriconazole and Posaconazole Prophylaxis [abstract]. https://atcmeetingabstracts.com/abstract/increase-in-potentially-resistant-non-aspergillus-molds-isolated-in-lung-transplant-recipients-after-voriconazole-and-posaconazole-prophylaxis/. Accessed February 16, 2026.« Back to 2018 American Transplant Congress
