Effect of HLA-DQ Mismatch on Efficacy Outcomes and Renal Function in Kidney Transplant Recipients: Subanalysis from the ELEVATE Study.
1ELEVATE Study Group, Köln, Germany
2Novartis Pharma AG, Basel, Switzerland
Meeting: 2017 American Transplant Congress
Abstract number: D67
Keywords: Efficacy, HLA matching, Kidney transplantation, Renal function
Session Information
Session Name: Poster Session D: Kidney Immunosuppression: Novel Regimens and Drug Minimization
Session Type: Poster Session
Date: Tuesday, May 2, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Purpose: Human leukocyte antigen (HLA)-DQ mismatches are often associated with acute rejection, independent of mismatches at other loci. Previous analysis from the ELEVATE (NCT01114529) study showed the effect of HLA-DR mismatch on renal allograft outcomes in kidney transplant recipients (KTxRs). Here, we present the effect of split and broad HLA-DQ mismatch on efficacy and safety in KTxRs receiving everolimus (EVR) vs standard calcineurin inhibitor (CNI).
Methods: ELEVATE was a 24-month (M), multicenter, open-label study, in which de novo KTxRs were randomized at 10-14 weeks post-kidney transplant (KTx) to receive EVR (n=360; C0: 6-10 ng/mL) or continue CNI regimen (n=357; tacrolimus [TAC] C0: 5-10 ng/mL; cyclosporine [CsA] C0: 100-250 ng/mL). Donor-recipient HLA-DQ mismatches were determined for split or broad categories. Composite efficacy failure (CEF; treated biopsy-proven acute rejection, graft loss, or death), acute rejection (AR), and antibody-mediated rejection (AMR) at M24 post-Tx were assessed. Renal function was assessed as estimated glomerular filtration rate (eGFR, MDRD4).
Results: Overall, 64 and 79 patients had split mismatch and 27 and 23 patients had broad mismatch in the EVR and CNI arm, respectively. At M24, CEF, AR, and AMR events were numerically higher in EVR vs CNI arm for split mismatch. However, for broad mismatch, all efficacy events were comparable between both the arms. eGFR was numerically higher in EVR vs CNI arm for both split and broad mismatch groups [Table]. Moreover, eGFR was significantly higher in EVR vs CsA arm for split mismatch group (P<0.05). Adverse events (AEs)/serious AEs were comparable between both arms. AEs/infections leading to discontinuation were higher in EVR vs CNI arm (split mismatch: 33.3% vs 13.8%; broad mismatch: 25.9% vs 13.0%).
Conclusion: EVR appears to offer better renal function despite higher efficacy failure and safety events vs CNI irrespective of the presence of split or broad mismatch at HLA-DQ loci. Assessment with larger samples is warranted to confirm these findings.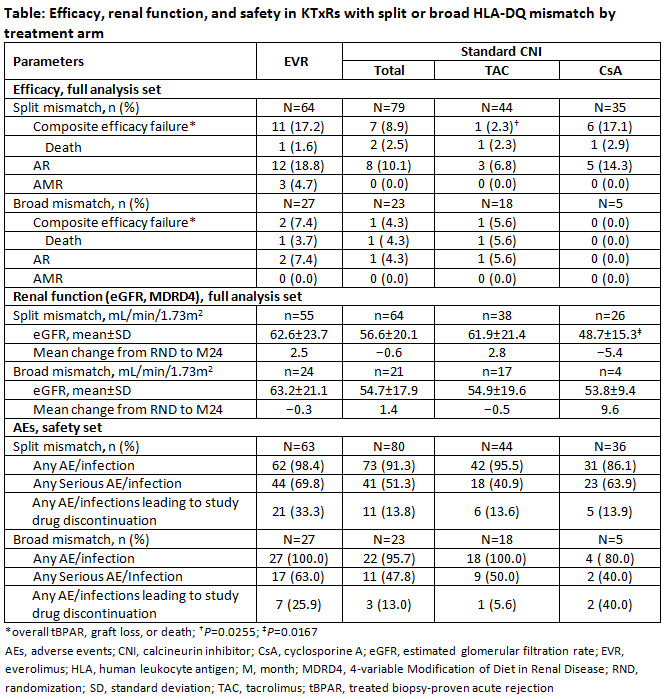
CITATION INFORMATION: Arns W, Cruzado J, Holdaas H, Lopez P, Bernhardt P, Bader G, Claas F, van der Giet M, de Fijter J. Effect of HLA-DQ Mismatch on Efficacy Outcomes and Renal Function in Kidney Transplant Recipients: Subanalysis from the ELEVATE Study. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Arns W, Cruzado J, Holdaas H, Lopez P, Bernhardt P, Bader G, Claas F, Giet Mvander, Fijter Jde. Effect of HLA-DQ Mismatch on Efficacy Outcomes and Renal Function in Kidney Transplant Recipients: Subanalysis from the ELEVATE Study. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/effect-of-hla-dq-mismatch-on-efficacy-outcomes-and-renal-function-in-kidney-transplant-recipients-subanalysis-from-the-elevate-study/. Accessed February 5, 2026.« Back to 2017 American Transplant Congress
