A Novel Technique to Increase Donor Utilization: Our Experience Using High-Dose Tissue Plasminogen Activator Flush in Donation-After-Cardiac-Death Donors for Liver Transplantation.
Surgery, Montefiore Medical Center, Bronx, NY
Meeting: 2017 American Transplant Congress
Abstract number: C83
Keywords: Donors, Liver grafts, Liver transplantation, marginal, non-heart-beating
Session Information
Session Name: Poster Session C: Donor Management: All Organs
Session Type: Poster Session
Date: Monday, May 1, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
The utilization of donation-after-cardiac-death (DCD) livers remains generally low. Strategies to address the perceived liabilities associated with DCD organs could influence their utilization in a positive direction. In our DCD donor surgical technique, tissue plasminogen activator (tPA) is added to normal saline and used as the initial in situ flush after the requisite no-touch period. In brief, 100 mg of lyophilized tPA is reconstituted in 100 mL of sterile water and then diluted in 1 L of room-temperature normal saline. DCD procurement follows the standard protocol in which the donor is terminally extubated and given 30,000 units of intravenous heparin. After asystole and a 5-minute no-touch period, the aorta is emergently cannulated, and tPA infusion is begun with concomitant cross-clamping of the thoracic aorta. The abdominal organs are flushed with cold University of Wisconsin (UW) solution until the effluent is clear. The organs are removed in the usual fashion. 13 DCD liver grafts were procured using this technique. The mean donor age was 26 years (range 12-48 years), and the mean donor warm ischemic time was 22 minutes (range, 19-30 min). Seven recipients had a mean Model for End-Stage Liver Disease (MELD) score 19 (no exception points). Six patients had MELD exception points (mean 28.5). 10 patients had no post-transplant biliary complications. One patient developed biliary ischemic cholangiopathy due to hepatic artery thrombosis. Another patient developed a mild extrahepatic biliary anastomotic stricture, but has never required intervention and is more than a year post-transplant. One patient died secondary to primary non-function due to macrosteatosis. High-dose normothermic tPA flush may be a viable strategy to reliably reduce ischemic cholangiopathy in DCD donor liver grafts and should be studied in a larger cohort.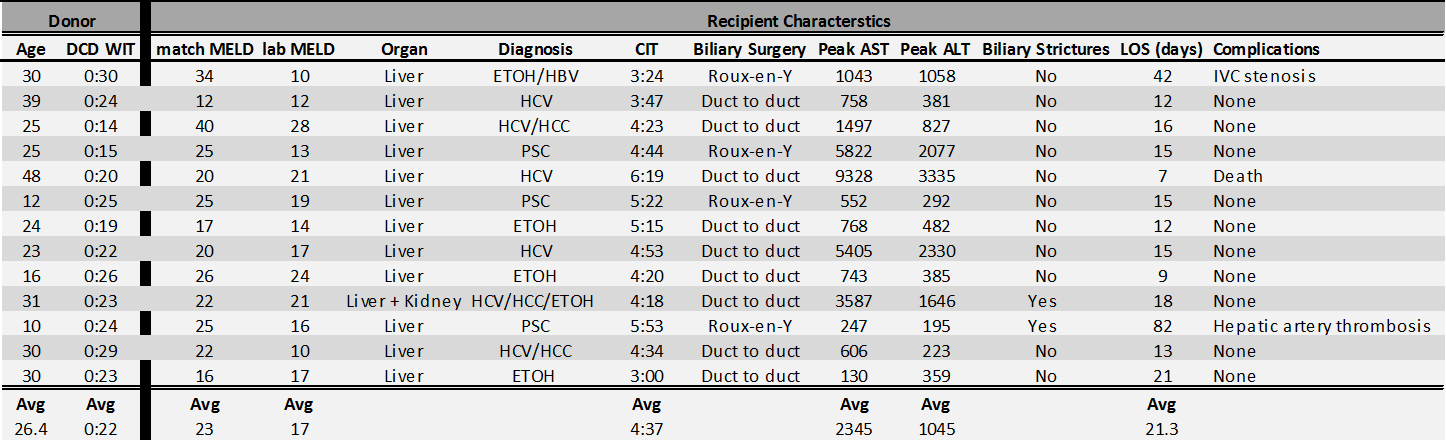
CITATION INFORMATION: Graham J, Lorenzen K, Bellemare S, Kinkhabwala M, Rocca J. A Novel Technique to Increase Donor Utilization: Our Experience Using High-Dose Tissue Plasminogen Activator Flush in Donation-After-Cardiac-Death Donors for Liver Transplantation. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Graham J, Lorenzen K, Bellemare S, Kinkhabwala M, Rocca J. A Novel Technique to Increase Donor Utilization: Our Experience Using High-Dose Tissue Plasminogen Activator Flush in Donation-After-Cardiac-Death Donors for Liver Transplantation. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/a-novel-technique-to-increase-donor-utilization-our-experience-using-high-dose-tissue-plasminogen-activator-flush-in-donation-after-cardiac-death-donors-for-liver-transplantation/. Accessed January 15, 2026.« Back to 2017 American Transplant Congress
