Safety of Liver Donation from Living Donors with Sickle Cell Trait.
H. Elsiesy,1,2 M. Sturdevant,1 W. Al-Hamoudi,1 H. Elbeshbeshy,1 M. Al Sebayel,1 A. Jaafari,1 F. Abaalkhail.1,2
1Liver Trasplantation, King Faisal Specialist Hospital &
Research Center, Riyadh, Saudi Arabia
2Medicine, Alfaisal University, Riyadh, Saudi Arabia
3Gastroenterology, King Saud University, Riyadh, Saudi Arabia
Meeting: 2017 American Transplant Congress
Abstract number: B227
Keywords: Liver transplantation, Living-related liver donors, Safety
Session Information
Session Name: Poster Session B: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Sunday, April 30, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Background:
Living donor liver transplant (LDLT) is an important source of organs particularly with the cadaveric organ shortage. It is the main source of liver transplant in the East. At our program, 63.6% of liver transplant were performed from LDLT (599 out of 941).
Donor safety is the main focus of donor evaluation. There is limited data on the safety of use of living liver donors in patient's sickle cell trait. We used to exclude donors with sickle cell trait but we started accepting them since 2012. We report the donor safety of 7 patients with sickle cell trait.
Methods:
This is a retrospective chart review of living liver donors from January 2012 until September 2016, seven donors identified. The medical records were reviewed for age, gender, relation to the recipient, Body mass index (BMI), blood group, history of preoperative blood transfusion to decrease Hemoglobin S (Hb S), Hemoglobin level, Mean corpuscular volume, Hb S level, hospital stay and complications.
Result:
Out of 7 donors, five were males , age between 24-38 (mean 30), all donors donated left lateral segment to a pediatric recipients, Hb level ranged from 11.3 to 16 (average 13.6), MCV ranged from 59-84 (70.3), Hb S level ranged from 21.2 to 36 (28.7), hospital stay from 4-6 days (average 4.8 days)
Two patients received blood transfusion 2 days prior to surgery and their Hb S level decreased from 32.8 and 36 to 27.5 and 30.6 respectively
All other patients donated blood 2 days before surgery and were well hydrated the day of surgery
2 patients has hypertrophic scar, one has peri-hepatic fluid collection and one has pelvic fluid collection that resolved spontaneously, otherwise no immediate or long-term complication related to the surgery or sickle cell trait.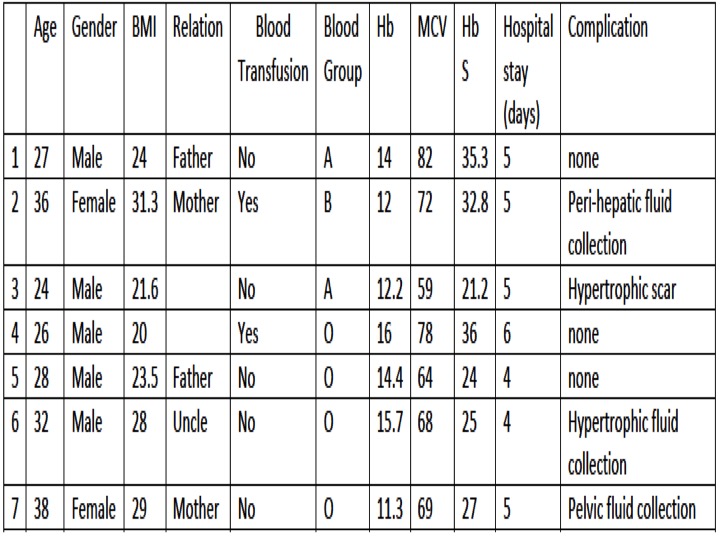 Conclusion:
Conclusion:
Liver donation is safe from sickle cell trait donors as long as dehydration is avoided and oxygen saturation is maintained normal throughout surgery. To our knowlege, this is the first series reporting safety in donor with sickle cell trait.
CITATION INFORMATION: Elsiesy H, Sturdevant M, Al-Hamoudi W, Elbeshbeshy H, Al Sebayel M, Jaafari A, Abaalkhail F. Safety of Liver Donation from Living Donors with Sickle Cell Trait. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Elsiesy H, Sturdevant M, Al-Hamoudi W, Elbeshbeshy H, Sebayel MAl, Jaafari A, Abaalkhail F. Safety of Liver Donation from Living Donors with Sickle Cell Trait. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/safety-of-liver-donation-from-living-donors-with-sickle-cell-trait/. Accessed January 5, 2026.« Back to 2017 American Transplant Congress
