Recovery from Hypophosphatemia as a Predictor of Post-Operative Morbidity in Live Donor Hepatectomy.
O. Serrano,1 D. Berglund,1 V. Goduguchinta,1 A. Reddy,1 J. Menk,2 D. Vock,3 V. Kirchner,1 R. Kandaswamy,1 A. Matas,1 T. Pruett,1 S. Chinnakotla.1
1Surgery, University of Minnesota, Minneapolis, MN
2Biostatistical Design and Analysis Center, Clinical and Translational Science Institute, Minneapolis, MN
3Biostatistics, School of Public Health, Minneapolis, MN
Meeting: 2017 American Transplant Congress
Abstract number: B225
Keywords: Liver transplantation, Living-related liver donors, Morbidity, Post-operative complications
Session Information
Session Name: Poster Session B: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Sunday, April 30, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
OBJECTIVE: Live donor hepatectomy (LDH) is associated with significant post-operative hypophosphatemia (POH), which is associated with liver regeneration. We investigated whether the rate of recovery from POH can be a surrogate marker for post-operative liver-specific morbidity (LSM).
METHODS: From January 1997 to April 2016, we performed 169 LDH for transplantation. Cohorts were defined by the presence of LSM (biliary leak, stricture, bleed) within 30 days of surgery. The linear slope of POH recovery was evaluated using a generalized linear model. Robust standard errors were computed using generalized estimating equations. Long-term complications (>30 days) were compared among the cohorts using a binomial regression.
RESULTS: Of the 169 LDH patients in our study, 15 (8.9%) suffered LSM. Baseline demographic characteristics, intraoperative time, estimated blood loss, or post-operative mortality were not statistically distinct between the LSM and non-LSM (NLSM) cohorts. The minimum phosphorus level (Pmin) was similar in both cohorts (1.75+0.55 mg/dl for LSM vs 1.94+0.57 mg/dl for NLSM) but the timing of Pmin appeared to be delayed for the LSM cohort (Fig. 1A). Furthermore, the rate of recovery from a hypophosphatemic insult trended faster for LSM than NLSM (Fig. 1B; p=0.06). Although liver enzyme recovery was indistinguishable among the cohorts, bilirubin (Fig. 1C) and INR (Fig. 1D) recovery in the LSM group was significantly dampened. Long-term complications were 5.1 times greater in the LSM than NLSM cohort (p = 0.04).
CONCLUSION: A rapid rate of recovery from POH after LDH is a surrogate marker for post-operative LSM and should warrant increased surveillance given risk of long-term complications.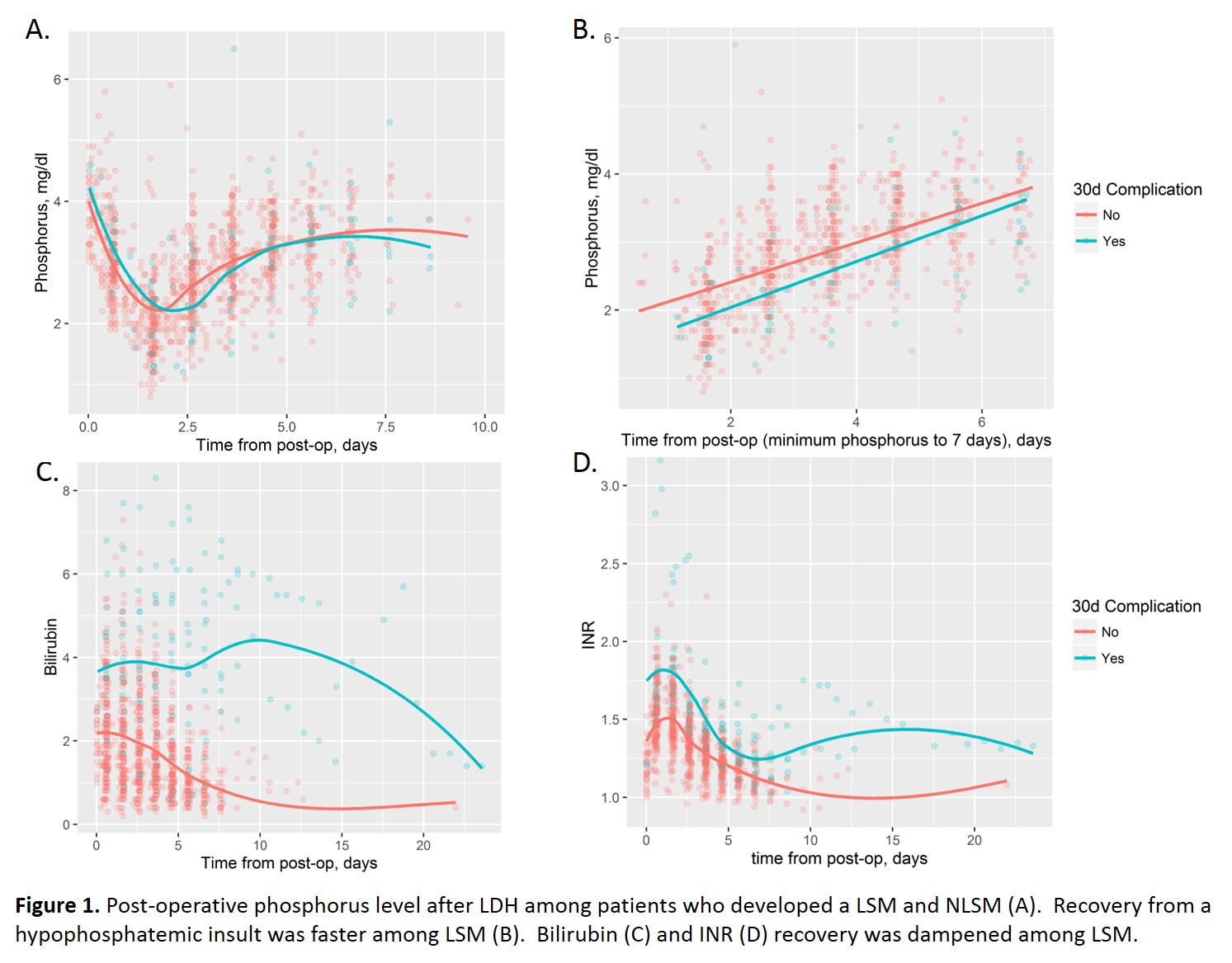
CITATION INFORMATION: Serrano O, Berglund D, Goduguchinta V, Reddy A, Menk J, Vock D, Kirchner V, Kandaswamy R, Matas A, Pruett T, Chinnakotla S. Recovery from Hypophosphatemia as a Predictor of Post-Operative Morbidity in Live Donor Hepatectomy. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Serrano O, Berglund D, Goduguchinta V, Reddy A, Menk J, Vock D, Kirchner V, Kandaswamy R, Matas A, Pruett T, Chinnakotla S. Recovery from Hypophosphatemia as a Predictor of Post-Operative Morbidity in Live Donor Hepatectomy. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/recovery-from-hypophosphatemia-as-a-predictor-of-post-operative-morbidity-in-live-donor-hepatectomy/. Accessed February 5, 2026.« Back to 2017 American Transplant Congress
