Predictive Value of Post Reperfusion TEG in Peri-Operative Outcomes During Liver Transplant.
Transplant Surgery, Hartford Hospital, Hartford, CT
Meeting: 2017 American Transplant Congress
Abstract number: B203
Keywords: Graft function, Morbidity
Session Information
Session Name: Poster Session B: Liver Retransplantation and Other Complications
Session Type: Poster Session
Date: Sunday, April 30, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Liver transplantation (LT) is the main treatment for patients with end-stage liver disease. During a liver transplant, persistent coagulations defects and fibrinolysis can be an early prediction of poor graft function. Patients with early allograft dysfunction (EAD) have been known to experience more problems such as a higher mortality and graft loss rates. They also tend to experience a longer ICU and hospital stay as well as increased postoperative complications. By using TEG we are able to monitor coagulation and TEG guided blood therapy during liver transplantation. We hypothesized that post reperfusion TEG can be a predictor of early graft function and clinical outcomes such as need for blood transfusions, reoperations, ICU stay and hospital LOS as well as need for retransplant and mortality. We reviewed the charts of 72 patients who underwent transplant from January 2012 to May 2016. We excluded patients who had no TEGs performed within 75 minutes after portal vein reperfusion. Pt's with post reperfusion fibrinolysis (>8%) were compared to those who had no fibrinolysis. There were 56 patient charts available for analysis: 42 had no evidence of fibrinolysis after reperfusion (28 +/- 18 minutes), 14 had fibrinolysis (20+/- 14 minutes, p=NS). There was no difference between the two groups in term of donor age, gender, DRI, recipient age, gender, MELD score, and warm or cold ischemic times. Pt's who had fibrinolysis required significantly more PRBC (17+/- 11 vs 9.79 +/-, p = 0.03) platelets (1.8 +/- 4 vs 3 +/- 3, p = 0.18) as well as more transfusion during the total hospital stay PRBC (18+/-13 vs 10+/-10, p=0.041), platelets (4 +/-4 vs 1 +/-4, p=0.006). Peak post op AST was also significantly higher in patients with fibrinolysis (3458 +/-3143 vs 1445 +/-1533, p=0.006) as well as in increase in ICU LOS. There was no difference in patient or graft survival although the two patients who developed primary non function that led to retransplant had evidence of post reperfusion fibrinolysis. Post reperfusion fibrinolysis is an early indicator of reperfusion injury and a possible sign of early graft dysfunction.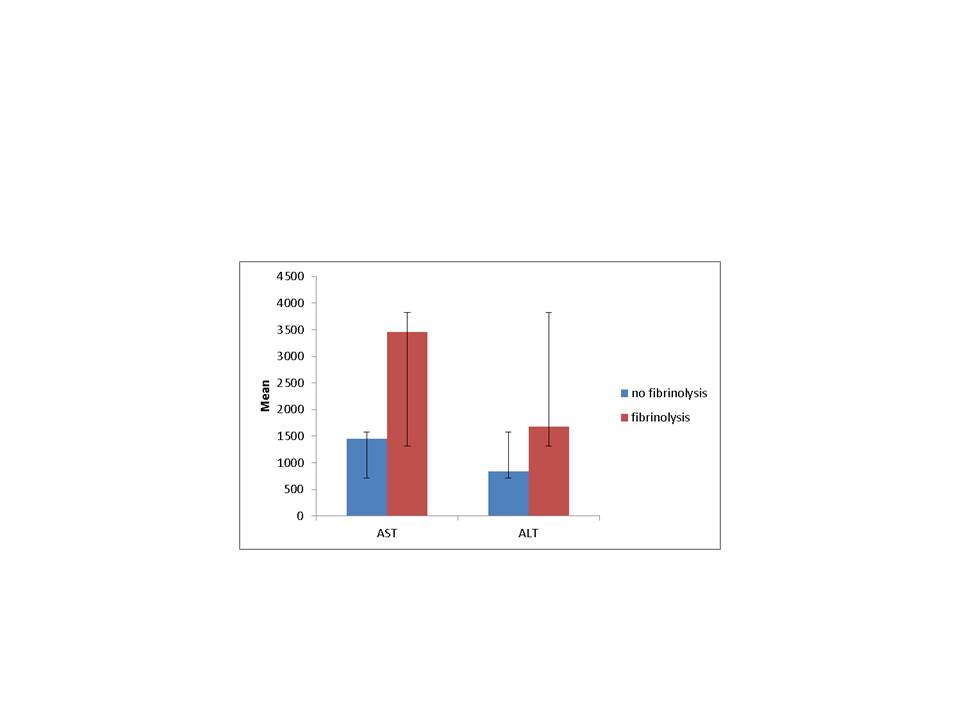
CITATION INFORMATION: Sheiner P, Sulejamnovic A, Salm J, Silver E, Rochon C. Predictive Value of Post Reperfusion TEG in Peri-Operative Outcomes During Liver Transplant. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Sheiner P, Sulejamnovic A, Salm J, Silver E, Rochon C. Predictive Value of Post Reperfusion TEG in Peri-Operative Outcomes During Liver Transplant. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/predictive-value-of-post-reperfusion-teg-in-peri-operative-outcomes-during-liver-transplant/. Accessed March 5, 2026.« Back to 2017 American Transplant Congress
