Clinical Outcomes of ABO and HLA Incompatible Kidney Transplantation – Nationwide Cohort Study.
1Transplantation Research Center, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
2Division of Nephrology, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
Meeting: 2017 American Transplant Congress
Abstract number: 533
Keywords: Highly-sensitized, HLA antibodies, Kidney transplantation
Session Information
Session Name: Concurrent Session: Long Term Kidney Graft Survival II
Session Type: Concurrent Session
Date: Tuesday, May 2, 2017
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:06pm-5:18pm
Presentation Time: 5:06pm-5:18pm
Location: E450a
Background This is a nationwide cohort study to investigate the impact of anti-A/B antibody or donor specific anti-HLA antibody (HLA-DSA) on the clinical outcomes in kidney transplant recipients (KTRs).
Methods Total 1,964 KTRs were included and we classified them into 4 groups; KTRs from ABO incompatible donor (ABOi, n=248); KTRs who had HLA-DSA (HLAi, n=144); combined ABOi and HLAi (ABOi+HLAi group, n=31); and the control group without ABOi or HLAi (CONT, n=1541). 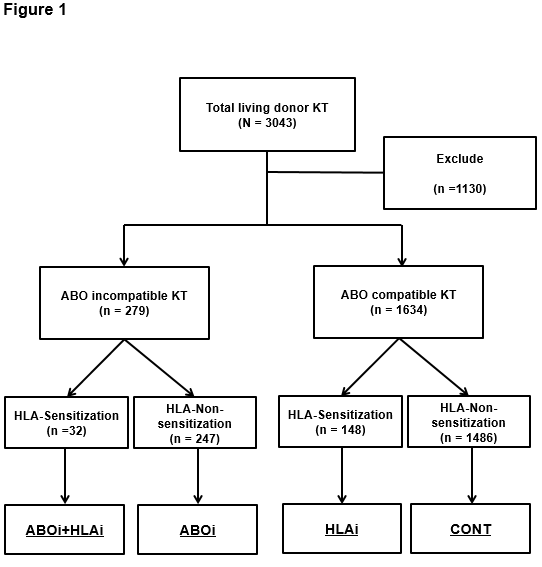 We compared post-transplant clinical outcomes such as the incidence of biopsy proven acute rejection (BPAR), allograft and patient survival rate among four groups.
We compared post-transplant clinical outcomes such as the incidence of biopsy proven acute rejection (BPAR), allograft and patient survival rate among four groups.
Results Incidence of BPAR was higher in the HLAi or ABOi+HLAi group than in the CONT group. In contrast, it was not higher in the ABOi group than the CONT group.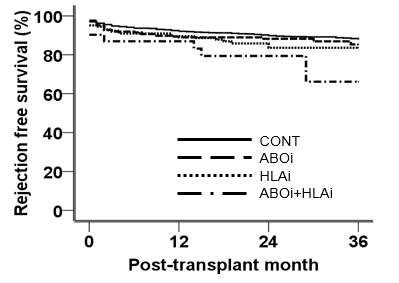 In addition, HLAi was a significant risk factor for BPAR in multivariate analysis, but ABOi was not. Death-censored graft survival rate did not differ across four groups. However, patient survival rate was lower in the ABOi group and ABOi+HLAi group than the CONT group and the most common cause of death in the former two groups were infection. Furthermore, multivariate analysis revealed that either desensitization due to ABOi or HLAi was independent risk factor for patient death.
In addition, HLAi was a significant risk factor for BPAR in multivariate analysis, but ABOi was not. Death-censored graft survival rate did not differ across four groups. However, patient survival rate was lower in the ABOi group and ABOi+HLAi group than the CONT group and the most common cause of death in the former two groups were infection. Furthermore, multivariate analysis revealed that either desensitization due to ABOi or HLAi was independent risk factor for patient death.
Conclusion HLAi was more important risk factor for BPAR than ABOi. However, pre-transplant desensitization because of either ABOi or HLAi significantly increased the risk for infection related mortality; hence effort to decrease infection is important for those patients to improve patient outcome.
CITATION INFORMATION: Ko E, Yu J, Yang C, Chung B, Korean Organ Transplantation Registry (KOTRY) Clinical Outcomes of ABO and HLA Incompatible Kidney Transplantation – Nationwide Cohort Study. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Ko E, Yu J, Yang C, Chung B. Clinical Outcomes of ABO and HLA Incompatible Kidney Transplantation – Nationwide Cohort Study. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/clinical-outcomes-of-abo-and-hla-incompatible-kidney-transplantation-nationwide-cohort-study/. Accessed February 7, 2026.« Back to 2017 American Transplant Congress
