Center Volume Does Not Influence the Risk Associated with Using High DRI Donor Livers.
1Department of Surgery, OSUWMC, Columbus, OH
2Department of Internal Medicine, OSUWMC, Columbus, OH
3Department of Internal Medicine, OSUWMC, Columbus, OH
4Department of Anesthesiology and Pain Medicine, Nationwide Children's Hospital, Columbus, OH
Meeting: 2017 American Transplant Congress
Abstract number: 459
Keywords: Donors, Liver transplantation, marginal
Session Information
Session Name: Concurrent Session: Optimizing Donor Utilization: All Organs
Session Type: Concurrent Session
Date: Tuesday, May 2, 2017
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:42pm-3:54pm
Presentation Time: 3:42pm-3:54pm
Location: E353B
Background: High risk donor allografts potentially reduce survival after liver transplantation (LT), but increase access. We evaluated whether differences in patient mortality associated with using high donor risk index (DRI) allografts for LT varied according to centers' annual number performed.
Methods: The UNOS registry was queried for LT performed 2/2002-12/2015 for adult, first-time recipients of whole LT alone. 1-year patient survival was the primary endpoint. Survival according to donor risk was compared in small and large centers (averaging <40 vs. ≥40 LT/year). Hazard ratio (HR) of high (DRI>1.9) vs. low donor risk was estimated using Cox regression. Donor risk was interacted with annual center volume, defined as total LT performed in a calendar year and the model was adjusted for relevant recipient factors. Predicted HR of high donor risk (representing excess mortality hazard attributable to using high as opposed to low risk donors) was plotted over the continuous measure of center volume.
Results: 45,343 patients were included (3,921 [9%] deceased within 1 year). In 67 small and 65 large centers, log-rank tests indicated greater mortality with high-DRI allografts (p<0.01). In multivariable analysis, high-DRI allografts predicted increased mortality hazard at centers performing 20 LT in a given year (HR=1.34; 95% CI: 1.20, 1.49; p<0.001) and, similarly, at centers performing 70 LT in a given year (HR=1.31; 95% CI: 1.22, 1.40; p<0.001). The interaction between high DRI and center volume was not significant (p=0.484), indicating that the hazard associated with high-DRI LT did not differ according to center volume 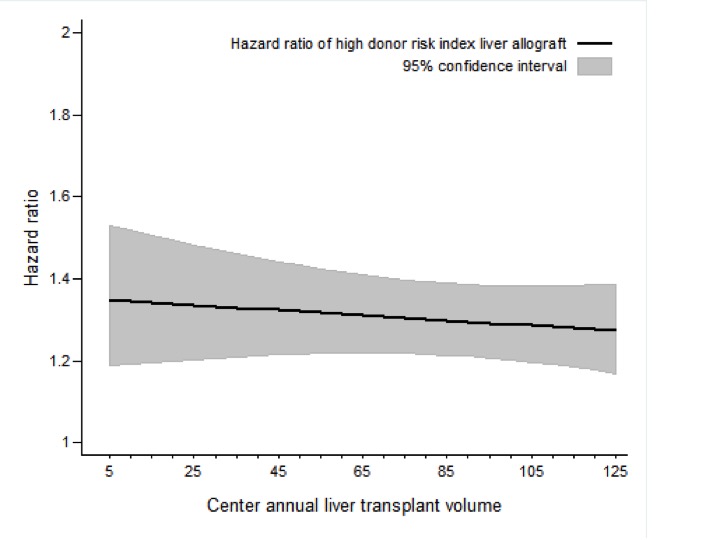 .
.
Conclusions: At both small and large centers, high-risk donor allografts were associated with reduced patient survival after LT. The proportional increase in mortality hazard attributable to high-risk donor allografts was not reduced at more experienced centers.
CITATION INFORMATION: Black S, Beal E, Mumtaz K, Hayes Jr. D, El-Hinnawi A, Washburn K, Tumin D. Center Volume Does Not Influence the Risk Associated with Using High DRI Donor Livers. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Black S, Beal E, Mumtaz K, Jr DHayes, El-Hinnawi A, Washburn K, Tumin D. Center Volume Does Not Influence the Risk Associated with Using High DRI Donor Livers. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/center-volume-does-not-influence-the-risk-associated-with-using-high-dri-donor-livers/. Accessed March 4, 2026.« Back to 2017 American Transplant Congress
