Current Status of HIV-to-HIV Transplants in the United States.
1JHU, Baltimore, MD
2Mount Sinai, New York, NY
3NIH, Bethesda, MD
4NYU, New York, NY
Meeting: 2017 American Transplant Congress
Abstract number: 455
Keywords: HIV virus, Kidney transplantation, Liver transplantation
Session Information
Session Name: Concurrent Session: Optimizing Donor Utilization: All Organs
Session Type: Concurrent Session
Date: Tuesday, May 2, 2017
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:54pm-3:06pm
Presentation Time: 2:54pm-3:06pm
Location: E353B
The HIV Organ Policy Equity (HOPE) Act allows transplantation using organs from HIV-infected (HIV+) donors for HIV+ individuals in the United States under research protocols. We opened the HOPE in Action trial (NCT02602262) to evaluate the safety and efficacy of HIV+ deceased donor kidney and liver transplantation.
Methods: HIV+ transplant candidates without active opportunistic infections (OI) on antiretroviral therapy (ART) with HIV RNA <50 c/mL, CD4 >200 or >100 cells/ul (kidney and liver, respectively) were eligible. HIV+ deceased donors could not have an active OI. An effective post-transplant recipient ART regimen had to be justified based on donor HIV RNA and ART history.
Results: Between March and November 2016, 3 HIV+/HIV+ kidney transplants and 1 HIV+/HIV+ liver transplant were performed. The first HIV+ donor was a 35 year-old Caucasian women on ART with HIV RNA <20 c/mL and CD4 1683 cells/uL who died of drug intoxication. The second donor was a 46 year-old African American female on ART with HIV RNA 475 c/ml and CD4 1533 who died of stroke. 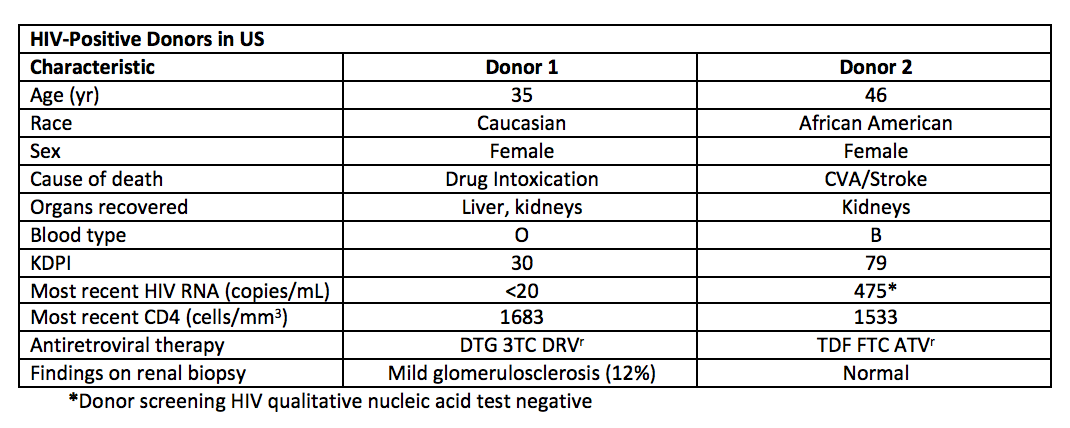 The first liver and kidney recipients are 8 months post-transplant; the third and fourth kidney recipients are 4 months post-transplant. There have been no episodes of graft rejection, failure, or HIV disease progression.
The first liver and kidney recipients are 8 months post-transplant; the third and fourth kidney recipients are 4 months post-transplant. There have been no episodes of graft rejection, failure, or HIV disease progression. 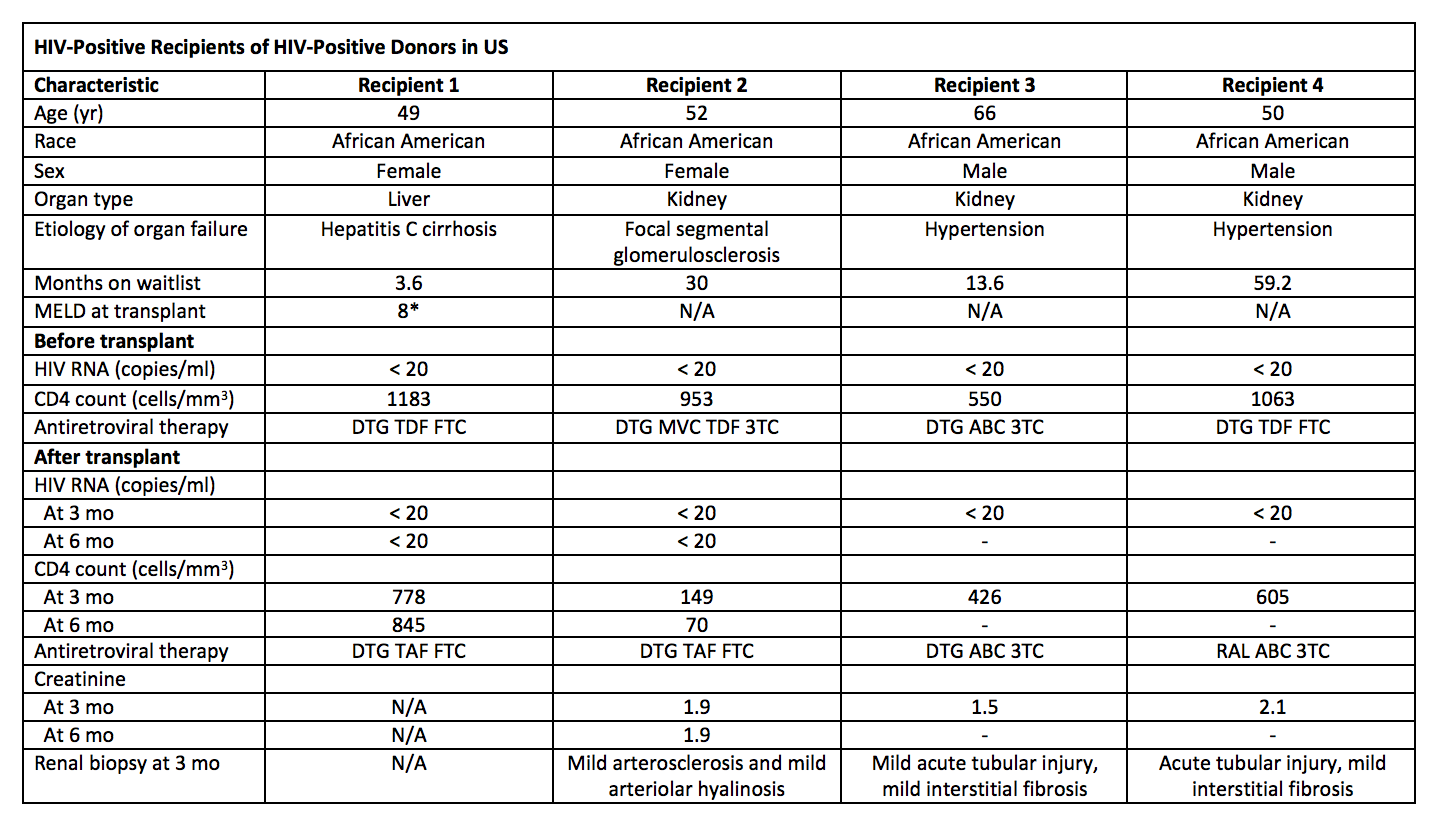 Conclusion: We report the first 4 successful cases of HIV+ to HIV+ transplants under the Congressional HOPE Act. These cases provide proof-of-concept that the use of HIV+ donors can increase access to organ transplants for HIV+ candidates who face high waitlist mortality.
Conclusion: We report the first 4 successful cases of HIV+ to HIV+ transplants under the Congressional HOPE Act. These cases provide proof-of-concept that the use of HIV+ donors can increase access to organ transplants for HIV+ candidates who face high waitlist mortality.
CITATION INFORMATION: Durand C, Tobian A, Desai N, Cameron A, Dagher N, Brown D, Halpern S, Bagnasco S, Ostrander D, Redd A, Huprikar S, Haydel B, Lerner S, Florman S, Segev D. Current Status of HIV-to-HIV Transplants in the United States. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Durand C, Tobian A, Desai N, Cameron A, Dagher N, Brown D, Halpern S, Bagnasco S, Ostrander D, Redd A, Huprikar S, Haydel B, Lerner S, Florman S, Segev D. Current Status of HIV-to-HIV Transplants in the United States. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/current-status-of-hiv-to-hiv-transplants-in-the-united-states/. Accessed February 20, 2026.« Back to 2017 American Transplant Congress
