Treating Ischemically Damaged Porcine Kidneys with Mesenchymal Stromal Cells During Normothermic Machine Perfusion.
1Surgery, UMCG, Groningen, Netherlands
2Internal Medicine, Erasmus Medical Center, Rotterdam, Netherlands
3Internal Medicine, UMCG, Groningen, Netherlands
4Nephrology, LUMC, Leiden, Netherlands
5Oxford Transplant Centre, University of Oxford, Oxford, United Kingdom
Meeting: 2017 American Transplant Congress
Abstract number: 213
Keywords: Kidney transplantation, Machine preservation, Stem cells
Session Information
Session Name: Concurrent Session: Emerging Interventions in Ischemia Reperfusion Injury
Session Type: Concurrent Session
Date: Monday, May 1, 2017
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:42pm-2:54pm
Presentation Time: 2:42pm-2:54pm
Location: E351
Normothermic machine perfusion (NMP) could provide superior organ preservation and offers the unique opportunity for interventions to an isolated kidney prior to transplantation. There is increasing evidence that mesenchymal stromal cells (MSCs) have a positive effect on ischaemia-reperfusion (IR) injury. However, in most studies MSCs are administered after transplantation, which exposes the whole patient to circulating cells. The purpose of this study was to determine whether administering MSCs during NMP is technically feasible, if MSCs remain viable, to which structures they home and which cytokines are secreted.
Porcine kidneys and autologous blood were obtained from slaughterhouses. Warm ischaemia time was 30 min and cold ischaemia time was 3.5-5 hrs. Kidneys were perfused in a recirculating circuit with autologous red blood cells, Williams' Medium E, albumin, creatinine and Augmentin during 6 hrs at 37[deg]C. After 1 h either 0, 10^5, 10^6 or 10^7 cultured human adipose tissue derived MSCs were added (n=3 per group). Perfusate and urine samples were taken regularly. Biopsies were taken to assess renal histology and to locate MSCs with immunohistochemistry. Luminex analysis was used to determine secretion products of MSCs.
During NMP, porcine kidneys were functional and produced urine. Infusing MSCs did not lead to detectable vascular emboli. After NMP, viable MSCs were found in the lumen of glomerular capillaries in the 10^7 MSC group (Figure 1), but not in the other groups. MSCs secreted pro-inflammatory cytokines IL-6, IL-8 and MCP-1 in response to the ischemically damaged kidney during NMP, in a dose-dependent fashion.
In conclusion, adding MSCs during pre-transplant renal NMP proved to be feasible. MSCs remained viable and detectable and secreted various pro-inflammatory cytokines. The minimum required MSC dose per kidney most likely lies between 10^6 and 10^7 cells.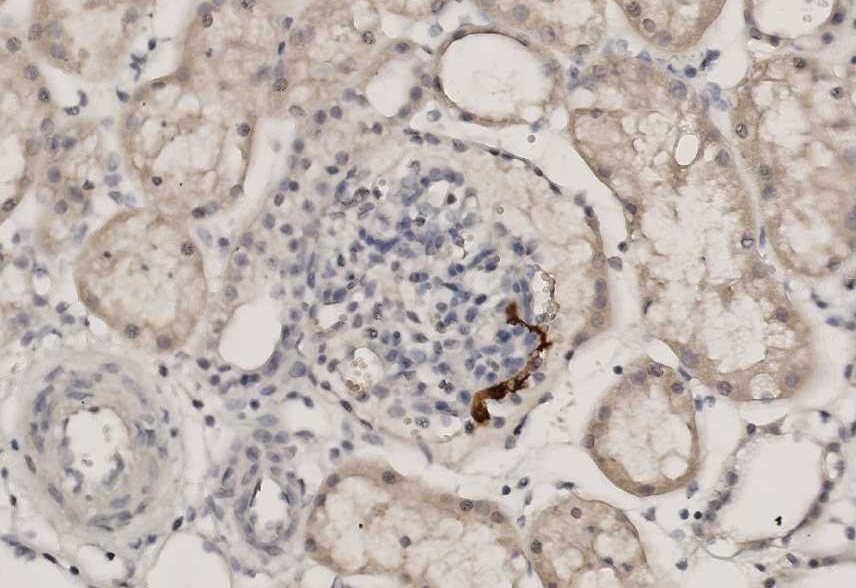
CITATION INFORMATION: Pool M, Sierra Parraga J, Roemeling-van Rhijn M, Reinders M, Hoogduijn M, Ploeg R, Leuvenink H, Moers C. Treating Ischemically Damaged Porcine Kidneys with Mesenchymal Stromal Cells During Normothermic Machine Perfusion. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Pool M, Parraga JSierra, Rhijn MRoemeling-van, Reinders M, Hoogduijn M, Ploeg R, Leuvenink H, Moers C. Treating Ischemically Damaged Porcine Kidneys with Mesenchymal Stromal Cells During Normothermic Machine Perfusion. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/treating-ischemically-damaged-porcine-kidneys-with-mesenchymal-stromal-cells-during-normothermic-machine-perfusion/. Accessed January 30, 2026.« Back to 2017 American Transplant Congress
