Are We Refusing Good Organs? Outcomes of Ventilator Management of Sub-Optimal Lung Donors.
1Congenital Heart Surgery, Texas Children's Hospital, Houston, TX
2Outcomes and Impact Services, Texas Children's Hospital, Houston, TX
3Pulmonology, Texas Children's Hospital, Houston, TX.
Meeting: 2016 American Transplant Congress
Abstract number: 24
Keywords: Donors, Lung transplantation, marginal, Pediatric
Session Information
Session Name: Concurrent Session: Donor Management: All Organs
Session Type: Concurrent Session
Date: Sunday, June 12, 2016
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:18pm-3:30pm
Presentation Time: 3:18pm-3:30pm
Location: Room 306
Purpose
Optimizing donor lung function is essential for organ acceptance and successful lung transplantation (LTx). We hypothesized that ventilator management of sub-optimal donor lungs, PaO2<300 mmHg, by the pediatric transplant pulmonologist on call would lead to equivalent recipient outcomes in the pediatric population.
Methods
Retrospective review of the UNOS database from 2010-2014 showed 936 lung donor offers at our institution and 75 LTx performed. To determine our donor management protocol effectiveness (changes to tidal volume, PEEP, and rate), LTx outcomes were compared between donors with a PaO2>300 vs. <300 mmHg at time of offer, and ventilator managed vs. non-managed donors. A univariate analysis was performed comparing baseline characteristics and recipient outcomes. Kaplan-Meier curves compared graft survival to date and freedom from bronchiolitis obliterans syndrome (BOS).
Results
Ventilator management occurred in 60/75 (80%) accepted donors. 9 (12%) had an initial PaO2 <300 mmHg and showed a median improvement of 119 mmHg (IQR 128.5) after management. There was no significant difference in donor characteristics or baseline recipient characteristics between groups. Recipient outcomes were similar between LTx from donors with initial PaO2>300 vs. <300 mmHg: there was no difference in primary graft dysfunction (grade=3) (17/66 (26%) vs. 4/9 (44%), p=0.26) or in acute cellular rejection (grade≥2) (10/66 (15.2%) vs. 1/9 (11.1%), p=1.0). There was also no difference in survival to date (p=0.74), or in freedom from BOS (p=0.99) between groups. Similar findings were observed when donors were grouped by ventilator managed vs. non-managed 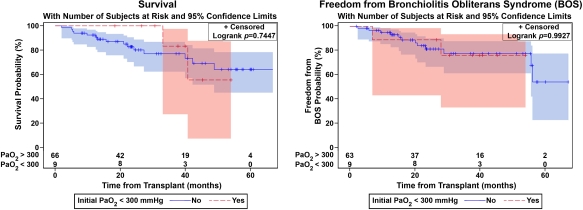 .
.
Conclusions
Sub-optimal lung donor offers are common (>10% of our center's accepted offers) and respond to ventilator management. This does not appear to negatively impact outcomes after LTx, suggesting that previously overlooked donors can be utilized in pediatric lung transplant recipients.
CITATION INFORMATION: Scully B, Horne D, Heinle J, McKenzie E, Hosek K, Zhang W, Mallory G, Melicoff E. Are We Refusing Good Organs? Outcomes of Ventilator Management of Sub-Optimal Lung Donors. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Scully B, Horne D, Heinle J, McKenzie E, Hosek K, Zhang W, Mallory G, Melicoff E. Are We Refusing Good Organs? Outcomes of Ventilator Management of Sub-Optimal Lung Donors. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/are-we-refusing-good-organs-outcomes-of-ventilator-management-of-sub-optimal-lung-donors/. Accessed February 5, 2026.« Back to 2016 American Transplant Congress
