Assessing the Impact of the Share35 Liver Allocation Policy: Survival Outcomes Among Liver Re-Transplant Recipients.
1Department of Surgery, University of Toledo, Toledo, OH
2George Mason University, Fairfax, VA
3Bucknell University, Lewisburg, PA.
Meeting: 2016 American Transplant Congress
Abstract number: 116
Keywords: Allocation, Liver grafts, Liver transplantation, Survival
Session Information
Session Name: Concurrent Session: Impact of New Allocation Systems and Novel Tools for Performance Enhancement in Abdominal Transplantation
Session Type: Concurrent Session
Date: Sunday, June 12, 2016
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:30pm-5:42pm
Presentation Time: 5:30pm-5:42pm
Location: Room 210
Liver retransplantation (reLTx) is the only treatment option for those who experienced graft loss after primary liver transplantation (LTx). Yet, in an era of increasing organ scarcity, the higher graft failure rate among reLTx recipients is a source of continuing controversy. Thus, this study uses the UNOS' liver transplant data (2011 -2015) to examine the survival outcomes in reLTx recipients with a MELD score of 35 and above after the share 35 liver allocation policy. Outcomes of interest are 1- and 2- year post-transplant graft and patient survivals.
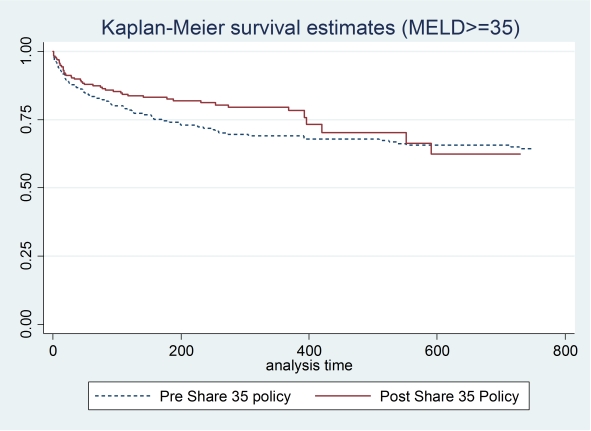
Kaplan-Meier estimates for the graft survivals at 1, 3, 6, 12, 36 months are 87.9%, 80.7%, 75.6%, 69.1%, and 64.3% in the MELD>=35 reLTx recipients before the policy. The estimates after the policy are 90.3%, 85.8%, 82.6%, 79.6%, and 62.4%. The log-rank test for equality of survivor functions demonstrates the significant improvement in 1-year graft survival among the reLTx recipients after the policy (p=0.03). There is no significant difference in 2-year graft survival before and after the policy (p=0.63). The estimates for the patient survivals are similar; they are 89.0%, 81.7%, 75.6%, 71.0% and 66.8% before the policy and 91.3%, 86.7%, 83.5%, 79.6% and 61.3% after the policy. The results of the log-rank tests are also similar, indicating significant improvement in 1-year patient survival since the policy (p=0.05) but no significant improvement in 2-year patient survival (p=0.28). Figure 1 presents the corresponding graft survival curves.
Cox-regression for graft failure also confirms the results. The hazard ratio of the interaction term between the share35 era and MELD>=35 patients is 0.64 (p=0.08). Donor risk index (DRI) is another significant variable for graft and patient survivals (p<0.001).
In conclusion, the share 35 policy seems to have improved 1-year graft and patient survivals in the reLTx recipients with a MELD score of 35 and over by about 10%. However, the policy did not seem to have improved 2-year survival outcomes in this cohort.
CITATION INFORMATION: Ortiz J, Koizumi N, Kwon C, Zhang Y, Ortiz C. Assessing the Impact of the Share35 Liver Allocation Policy: Survival Outcomes Among Liver Re-Transplant Recipients. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Ortiz J, Koizumi N, Kwon C, Zhang Y, Ortiz C. Assessing the Impact of the Share35 Liver Allocation Policy: Survival Outcomes Among Liver Re-Transplant Recipients. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/assessing-the-impact-of-the-share35-liver-allocation-policy-survival-outcomes-among-liver-re-transplant-recipients/. Accessed February 18, 2026.« Back to 2016 American Transplant Congress
