Conditional Long Term Intestine Patient and Graft Survival Is Improving Under rATG Immunosuppression in Pediatric Intestine Transplantation.
1Hillman Center for Pediatric Transplantation, Children's Hospital of Pittsburgh of UPMC, Pittsburgh, PA
2Intestinal Care and Rehabilitation Center, Children's Hospital of Pittsburgh of UPMC, Pittsburgh, PA.
Meeting: 2016 American Transplant Congress
Abstract number: 555
Keywords: Immunosuppression, Intestinal transplantation, Pediatric
Session Information
Session Name: Concurrent Session: Small Bowel Transplantation
Session Type: Concurrent Session
Date: Tuesday, June 14, 2016
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:06pm-5:18pm
Presentation Time: 5:06pm-5:18pm
Location: Room 102
Aim: We reviewed conditional graft survival and short and long term improvements in children receiving rATG (rabbit anti-thymocyte globulin) immunosuppression for intestine transplantation at a single center over 15 years. Methods: All children undergoing primary intestine transplantation under rATG and non rATG immunosuppression were analyzed. rATG immunosuppression was with 5 mg/kg rATG/ Tacrolimus/ Prednisolone (n=126) and other immunosuppression consisting of Tacrolimus/ Prednisolone (n=50), Tacrolimus/ Prednisolone/ Daclizumab (n=23), Tacrolimus/ Prednisolone/ Cyclophosphamide (n=16), Alemtuzumab (n=21) and Tacrolimus/ Prednisolone/ Basiliximab (n=1). Patients with intact grafts at one year were followed for subsequent long term outcomes of patient and graft survival, retransplant outcomes and significant morbidities. Results: 242 children underwent primary intestine transplantation between 1990 and 2015 consisting of isolated small bowel (n=94, 39%), liver and small bowel (n=109, 45%), modified multivisceral (n=7, 3%) and multivisceral type transplantations (n=32, 13%). The major causes of intestinal failure were gastroschisis (n=62, 26%), volvulus (n=51, 21%), necrotizing enterocolitis (n=28, 12%), pseudo obstruction (n=30, 12%), intestinal atresia (n=23, 10%) and microvillus inclusion disease (n=17, 7%). Conditional graft survival at 15 years for rATG and non rATG groups is illustrated in Figure 1. 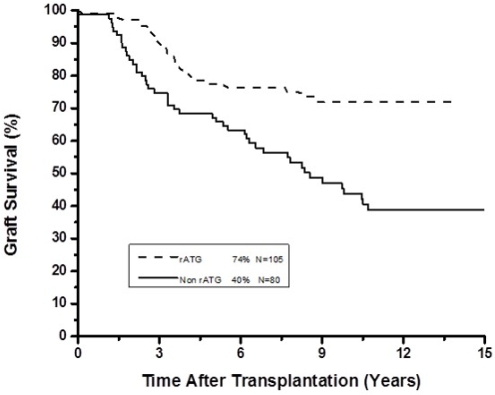 Patients with intact grafts at one year had the subsequent outcomes, stratified by rATG and non rATG immunosuppression in Table 1.
Patients with intact grafts at one year had the subsequent outcomes, stratified by rATG and non rATG immunosuppression in Table 1.
| Initial induction | rATG n |
non-rATG n |
| Patients | 126 | 111 |
| Intact grafts at one year | 105/126 (83%) | 80/111 (72%) |
| Alive with intact graft | 80 (76%) | 34 (43%) |
| Alive with retransplant | 7 | 5 |
| Alive with graft removed | 4 | 6 |
| Deceased | 17 | 37 |
| PTLD | 13/126 (10.3%) | 36/111 (32.4%) |
| Chronic rejection | 20/126 (16%) | 21/111 (19%) |
CITATION INFORMATION: Celik N, Vyas F, Bond G, Soltys K, Rudolph J, Sindhi R, Mazariegos G. Conditional Long Term Intestine Patient and Graft Survival Is Improving Under rATG Immunosuppression in Pediatric Intestine Transplantation. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Celik N, Vyas F, Bond G, Soltys K, Rudolph J, Sindhi R, Mazariegos G. Conditional Long Term Intestine Patient and Graft Survival Is Improving Under rATG Immunosuppression in Pediatric Intestine Transplantation. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/conditional-long-term-intestine-patient-and-graft-survival-is-improving-under-ratg-immunosuppression-in-pediatric-intestine-transplantation/. Accessed January 30, 2026.« Back to 2016 American Transplant Congress
