Intestinal Retransplantation in Children: Single Center Experience.
1Hillman Center for Pediatric Transplantation, Children's Hospital of Pittsburgh of UPMC, Pittsburgh, PA
2Intestinal Care and Rehabilitation Center, Children's Hospital of Pittsburgh of UPMC, Pittsburgh, PA.
Meeting: 2016 American Transplant Congress
Abstract number: 552
Keywords: Intestinal transplantation, Pediatric, Retransplantation
Session Information
Session Name: Concurrent Session: Small Bowel Transplantation
Session Type: Concurrent Session
Date: Tuesday, June 14, 2016
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:30pm-4:42pm
Presentation Time: 4:30pm-4:42pm
Location: Room 102
Aim: To analyze the patient and graft characteristics and improvement in patient outcomes for intestinal retransplantation (Re-ITx) in the era of induction immunosuppression with the comparison of outcomes between 1990-2000 and 2001-2015. Methods: The data of all children receiving Re-ITx between 1990 and 2015 at our center were reviewed retrospectively.Results: 242 children received primary intestinal grafts. 23 children (9.5%) were retransplanted with 24 grafts. Causes of graft failure were acute cellular rejection (n=3), liver failure (n=2), chronic rejection (n=11), post-transplant lymphoproliferative disorder (n=3), graft dysmotility or dysfunction (n=2), volvulus (n=1), arterial graft aneurysm (n=1), and aortic graft thrombosis (n=1). Re-ITx was with isolated small bowel in five, liver-small bowel±pancreas in five, multivisceral in thirteen and modified multivisceral in one. Sixteen (69.6%) patients are alive with functioning grafts at a mean current follow-up time of 8.8 years. 5 year patient and graft survival improved to 89% and 79% respectively since 2001. 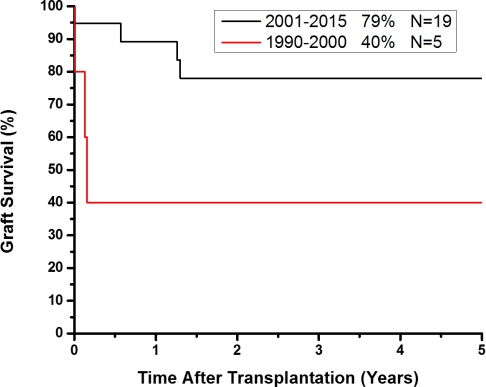 Seven patients died primarily from infectious complications at a mean time of 35.7 months post-Re-ITx. Two patients had allograft enterectomies due to severe acute rejection and chronic rejection. 93% of surviving patients with their retransplanted intestine weaned-off total parenteral nutrition and intravenous fluids. Conclusions: Improved early and intermediate term survival and outcome in pediatric Re-ITx may be attributed to improvements ininitial immunosuppression protocols, technical modifications, proper timing, and improved infectious disease monitoring. Careful patient selection and post-transplant management are essential for successful long-term outcome.
Seven patients died primarily from infectious complications at a mean time of 35.7 months post-Re-ITx. Two patients had allograft enterectomies due to severe acute rejection and chronic rejection. 93% of surviving patients with their retransplanted intestine weaned-off total parenteral nutrition and intravenous fluids. Conclusions: Improved early and intermediate term survival and outcome in pediatric Re-ITx may be attributed to improvements ininitial immunosuppression protocols, technical modifications, proper timing, and improved infectious disease monitoring. Careful patient selection and post-transplant management are essential for successful long-term outcome.
CITATION INFORMATION: Celik N, Vyas F, Bond G, Soltys K, Rudolph J, Sindhi R, Mazariegos G. Intestinal Retransplantation in Children: Single Center Experience. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Celik N, Vyas F, Bond G, Soltys K, Rudolph J, Sindhi R, Mazariegos G. Intestinal Retransplantation in Children: Single Center Experience. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/intestinal-retransplantation-in-children-single-center-experience/. Accessed February 10, 2026.« Back to 2016 American Transplant Congress
