Long Term Outcomes Following Antibody Mediated Rejection (AMR) in Renal Transplant Recipients.
Columbia University, New York.
Meeting: 2016 American Transplant Congress
Abstract number: D31
Keywords: HLA antibodies, Kidney transplantation, Outcome, Rejection
Session Information
Session Name: Poster Session D: Antibody Mediated Rejection: Session #2
Session Type: Poster Session
Date: Tuesday, June 14, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
INTRO: Progress in AMR treatment has improved early graft survival. Since the new kidney allocation system results in more sensitized patients getting transplanted, we expect AMR to continue to be a problem. However, data is scarce on long-term outcomes and which treatments improve survival.
METHODS: We reviewed our records at Columbia University Renal Transplant Program to identify AMR cases and collected data regarding type of txp, AMR treatment, response to therapy, patient/graft survival, and infectious complications.
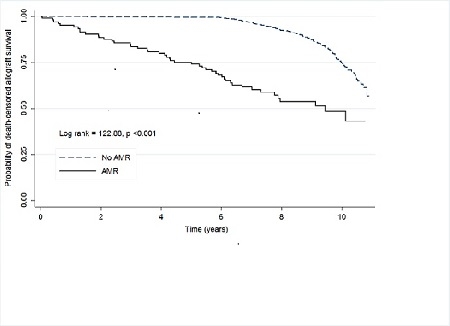
RESULTS: Between 2005 and 2009 we performed 1,209 adult renal txps, of whom 107 (8.9%) had AMR. The mean follow up in the AMR group was 5.7 yrs (4.2 yrs after rejection) compared to 8.3 yrs in the non-AMR controls. AMR cases more likely to be female (p<0.0001), younger (40.5 vs 50.1 yrs; p<0.0001), and a live donor recipient (57.3 vs. 46.6%; p = 0.0379). Time to AMR was 2.1 (IQR: 112.3) months with a mean creatinine of 3.86 ± 2.32. The majority of AMR patients (67.3%) received pheresis/IVIG/steroids, 26.2% received high dose IVIG/steroids, 4.7% received steroids alone, and the remaining 1.8% received increased baseline immunosuppression or no treatment. 11 patients also received rituximab.
Graft survival after AMR was 85.5% at 1 yr, and 59.3% at 5 yrs. Time to rejection (<6 months of txp: HR=1.45, NS), donor type (deceased: HR = 1.64, NS), treatment response (>25% decline in creatinine 1 month after AMR, HR 0.93, NS), and treatment type (PP/IVIG vs. IVIG: HR = 1.55, NS) were not associated with graft-failure. Rituximab did not affect graft loss(HR = 0.462, NS). Each 1 mg/dL increase in creatinine at time of AMR was associated with a 17.5% increased relative risk of graft loss(p=0.003). Compared to the non-AMR group, our AMR cohort were 3 times more likely to lose their allograft (OR 3.3, p <0.0001) but were less likely to die (OR = 0.03, p = 0.0007). Post-AMR treatment, 10% of patients developed BK viremia, while 6.5% had CMV disease.
CONCLUSION: Our data confirms other single center reports showing worse long-term renal outcomes after AMR. Despite improvements in short term outcomes, we need more effective therapy for AMR prevention and treatments.
CITATION INFORMATION: Crew R, Patel S, Morris H, Chiles M, Ratner L. Long Term Outcomes Following Antibody Mediated Rejection (AMR) in Renal Transplant Recipients. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Crew R, Patel S, Morris H, Chiles M, Ratner L. Long Term Outcomes Following Antibody Mediated Rejection (AMR) in Renal Transplant Recipients. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/long-term-outcomes-following-antibody-mediated-rejection-amr-in-renal-transplant-recipients/. Accessed February 14, 2026.« Back to 2016 American Transplant Congress
