Incidence of Post-Transplant Lymphoproliferative Disorder in First, Kidney-Only Transplant Recipients Remains Stable.
1Chronic Disease Research Group, Minneapolis
2Brystol-Myers Squibb Company (BMS), Hopewell
3BMS, Lawrenceville.
Meeting: 2016 American Transplant Congress
Abstract number: B305
Keywords: Kidney transplantation, Lymphoproliferative disease, Post-transplant lymphoproliferative disorder (PTLD), Risk factors
Session Information
Session Name: Poster Session B: PTLD/Malignancies: All Topics
Session Type: Poster Session
Date: Sunday, June 12, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
We estimated the incidence of and risk factors for post-transplant (TX) lymphoproliferative disorder (PTLD) in the 3 years post-TX for adults with first, kidney-only TX 2007-2012, and compared results with previously published work (Kasiske, et al. Am J Kidney Dis 2011; 58:970-980; study years 2000-2006). This retrospective cohort study used the US Renal Data System standard analytic file and Medicare claims. Patients were followed from TX until PTLD, return to dialysis, death, 3 years post-TX or Dec. 31, 2012. PTLD was identified from OPTN recipient follow-up forms and Medicare diagnosis codes. We estimated the relative risk (RR) of PTLD using a Cox proportional hazards model adjusted for recipient and donor characteristics.
Characteristics of the 74,959 patients we identified were similar to those of the 89,485 patients studied previously, except that our cohort was somewhat older (18% ages ≥65 vs 13%) and used more tacrolimus (88% vs 65%) and less cyclosporine (6% vs 27%). In OPTN data, PTLD incidence in the 3 years post-TX remained about 3.5 per 1000 person-years (PY), but incidence dropped (2.0 to 1.4 per 1000 PY) during the first year and increased (1.9 to 2.5 per 1000 PY) during years 2-3. In our study, among the approximately 50% of patients with complete Medicare coverage, PTLD incidence was 6.3 (95% CI: 5.5-7.2) during the first year post-TX and 3.1 (95% CI: 2.6-3.6) per 1000 PY during years 2-3. Using the full cohort and OPTN data, we identified risk factors for PTLD. RR for PTLD increased with age and decreased with more time between ESRD onset and TX. The risk was 4 times (RR: 4.4, 95% CI: 3.3-5.8) higher for patients who were EBV seronegative vs seropositive at TX; induction with IL-2RA was associated with a higher risk of PTLD compared with T-cell depleting antibodies. 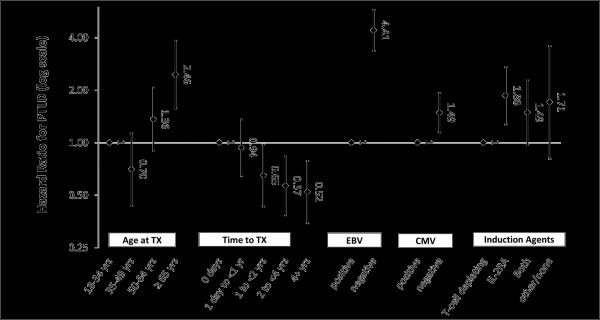 The previous work found similar patterns. Factors associated with PTLD remain similar and incidence has not changed substantially, but onset appears to be later, with fewer cases in the first year and more cases in years 2-3 post-TX.
The previous work found similar patterns. Factors associated with PTLD remain similar and incidence has not changed substantially, but onset appears to be later, with fewer cases in the first year and more cases in years 2-3 post-TX.
CITATION INFORMATION: Molony J, Peng Y, Baker N, Meier-Kriesche U, Snyder J. Incidence of Post-Transplant Lymphoproliferative Disorder in First, Kidney-Only Transplant Recipients Remains Stable. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Molony J, Peng Y, Baker N, Meier-Kriesche U, Snyder J. Incidence of Post-Transplant Lymphoproliferative Disorder in First, Kidney-Only Transplant Recipients Remains Stable. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/incidence-of-post-transplant-lymphoproliferative-disorder-in-first-kidney-only-transplant-recipients-remains-stable/. Accessed February 13, 2026.« Back to 2016 American Transplant Congress
