Outcomes in Lung Transplant Patients Requiring Extracorporeal Membrane Oxygenation (ECMO) in the Perioperative Period.
Cardiovascular Surger, Hospital of the University of Pennsylvania, Philadelphia, PA.
Meeting: 2016 American Transplant Congress
Abstract number: B288
Keywords: Lung transplantation, Mechnical assistance, Outcome, Risk factors
Session Information
Session Name: Poster Session B: Lung Transplantation Posters
Session Type: Poster Session
Date: Sunday, June 12, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Objective As ECMO therapy is increasingly used to bridge high-risk patients with end-stage respiratory failure to lung transplantation, outcomes of this strategy employed in the perioperative period are not well studied. We report outcomes of this high-risk cohort.
Methods From 2004 to 2014, the Pennsylvania Health Cost Containment Council (PHC4) database was retrospectively reviewed for single (SLT)/bilateral lung transplantations (BLT) and ECMO. 237 patients were identified (mean age 53.9±12.9, 42.6% female), 80.2% (n=190) required ECMO support post-transplant (Group 1), and 19.8% (n=47) were ECMO dependent pre-transplant (Group 2), of which 7 patients stayed on ECMO post-transplant. Groups were compared using descriptive statistics; a logistic regression model was constructed to identify risk factors for in-hospital and midterm mortality over a follow-up of 2 years.
Results Group 2 patients were younger (46.9±13.1 vs 55.7±12.3,p<0.01) with a higher frequency of cystic fibrosis (42.4% vs 7.3%, p<0.01). 100% of Group 2 patients underwent BLT compared to 84.2% in Group 1 (p=0.004). Median duration of pre-transplant ECMO was 6d (interquartile range 3-12d) with a higher proportion requiring prolonged ventilation (>96h) (51.1% vs 29.5%, p=0.005). Both in-hospital and midterm all-cause mortality was lower in Group 2 (10.6% vs 32.1%, p=0.003 and 19.1% vs 42.1%, p=0.004; 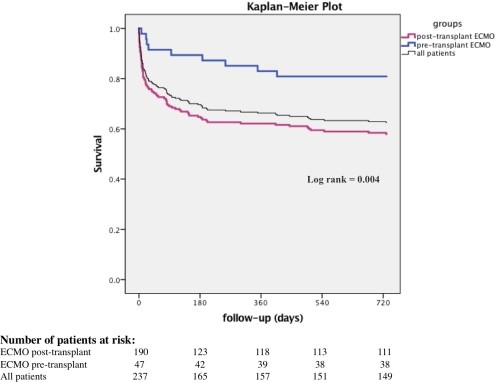 . Of 7 patients remaining on ECMO post-transplant, 14.3% died in-hospital. COPD was the prevalent etiology in group I patients (16.3% vs 2.1, p=0.011), mean hospital length of stay was 49.3±35.2d vs 61.9±26.2d, p=0.034. On logistic regression, age and post-transplant renal failure were independent risk factors for in-hospital (Odds Ratio OR=1.04 and OR=5.37) and midterm mortality (OR=1.03 and OR=2.24).
. Of 7 patients remaining on ECMO post-transplant, 14.3% died in-hospital. COPD was the prevalent etiology in group I patients (16.3% vs 2.1, p=0.011), mean hospital length of stay was 49.3±35.2d vs 61.9±26.2d, p=0.034. On logistic regression, age and post-transplant renal failure were independent risk factors for in-hospital (Odds Ratio OR=1.04 and OR=5.37) and midterm mortality (OR=1.03 and OR=2.24).
Conclusion Use of ECMO to bridge carefully selected patients to lung transplantation offers acceptable perioperative and midterm outcomes. Requirement for ECMO in the post-transplant period is associated with higher mortality. Age and renal failure are risk factors in this high-risk cohort.
CITATION INFORMATION: Habertheuer A, Williams M, Miller S, Cantu E, Bermudez C, Vallabhajosyula P. Outcomes in Lung Transplant Patients Requiring Extracorporeal Membrane Oxygenation (ECMO) in the Perioperative Period. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Habertheuer A, Williams M, Miller S, Cantu E, Bermudez C, Vallabhajosyula P. Outcomes in Lung Transplant Patients Requiring Extracorporeal Membrane Oxygenation (ECMO) in the Perioperative Period. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/outcomes-in-lung-transplant-patients-requiring-extracorporeal-membrane-oxygenation-ecmo-in-the-perioperative-period/. Accessed March 4, 2026.« Back to 2016 American Transplant Congress
