Donor Specific Antibody Used to Predict Crossmatch Results: A Clinically Useful Algorithm Derived from the College of American Pathologists Survey.
1Transplant Surgery, University of Vermont Medical Center, Burlington, VT
2Pathology, University of Vermont Medical Center, Burlington, VT.
Meeting: 2016 American Transplant Congress
Abstract number: B87
Keywords: Histocompatibility antigens, HLA matching
Session Information
Session Name: Poster Session B: Donor Management: All Organs
Session Type: Poster Session
Date: Sunday, June 12, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Purpose: While there are multiple modalities to perform a preoperative crossmatch for organ transplant surgery, the cytotoxic crossmatch remains the gold standard for detection of incompatible allografts. Solid phase immunoassays such as Luminex technology allow for virtual crossmatching, potentially decreasing cost and time in the preoperative evaluation. However the clinical reliability of the virtual crossmatch remains unclear.
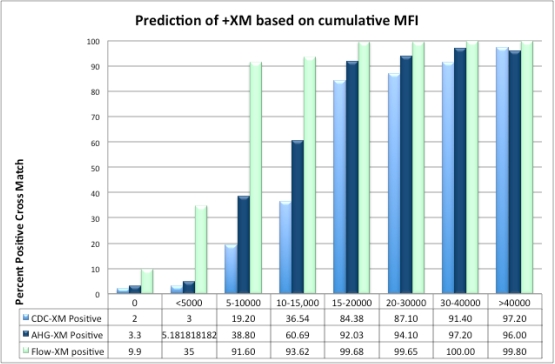
Methods: We performed a retrospective review of the College of American Pathologists HLA Surveys from 2011-2014, which are sent to transplant institutions as an accreditation tool. Each involves a standard sample of cells and serum tested using the preferred crossmatch approach of participating centers. These include direct complement-directed cytotoxicity, anti-human globulin (AHG) augmented, and flow cytometry. Our HLA laboratory performed solid phase immunoassay (Luminex) on all samples to detect for the presence of donor-specific antibodies (DSA), and quantified the relative strength and quantity of each DSA using the mean fluorescent intensity (MFI). Using these data, we compared the cumulative MFI to the national crossmatch results.
Results: A total of 144 survey results were analyzed over the time period. Direct, AHG, and flow crossmatches all had strong direct nonlinear correlation with the Luminex cumulative MFI (r2=0.8, 0.88, and 0.87 respectively). For MFI of 0, less than 5000, 5000-10,000, and 10,000-15,000, there were probabilities of a positive AHG-crossmatch of 3.3, 5.2, 38.8, and 60.7%, respectively.
Conclusions: We present an algorithm and predictive tool that can be replicated nationally at transplant centers that participate in the College of American Pathologists survey. Comparing DSA data on standardized anonymous blood samples against nationally performed crossmatches can help predict the probabilities of these laboratory outcomes, which may assist clinicians in the preoperative transplant workup.
CITATION INFORMATION: Wrenn S, Hain D.-S, Harm S, Hillyard S, Shah D, Hammond P, Marroquin C, Fung M. Donor Specific Antibody Used to Predict Crossmatch Results: A Clinically Useful Algorithm Derived from the College of American Pathologists Survey. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Wrenn S, Hain D-S, Harm S, Hillyard S, Shah D, Hammond P, Marroquin C, Fung M. Donor Specific Antibody Used to Predict Crossmatch Results: A Clinically Useful Algorithm Derived from the College of American Pathologists Survey. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/donor-specific-antibody-used-to-predict-crossmatch-results-a-clinically-useful-algorithm-derived-from-the-college-of-american-pathologists-survey/. Accessed March 7, 2026.« Back to 2016 American Transplant Congress
