Early De Novo DSA with T Cell Mediated Rejection (TCMR) Is Associated with Allograft Dysfunction with Chronic Injury.
UPMC, Pittsburgh.
Meeting: 2016 American Transplant Congress
Abstract number: A50
Keywords: Alloantibodies, Graft function, Rejection
Session Information
Session Type: Poster Session
Date: Saturday, June 11, 2016
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Halls C&D
De novo anti-donor HLA specific antibody (DSA) detected post-renal transplantation is associated with adverse outcomes. However, the relationship between early de novo DSA and subsequent TCMR and its impact is unknown. In this prospective longitudinal study, DSA was measured at 0, 1, 3, 6, 9, 12 & 18m post Tx and compared to the development of TCMR on protocol (3m & 12m) and for-cause biopsies, and subsequent outcomes were assessed.
53 (18%) of 299 patients transplanted between dates 1/13 and 7/14 developed de novo DSA (IS:Thymo, MPA+TAC & rapid steroid withdrawal). In 48/53 (90%) of these patients, DSA developed early (<6m). Importantly, 20/53 (38%) patients had DSA prior to, or concomitant with, clinical/sub-clinical TCMR. Whereas 4 patients developed DSA after TCMR. 3 patients had ABMR and were excluded.
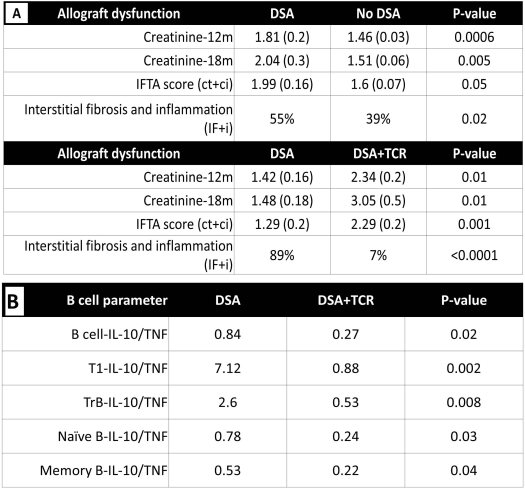
Patients with de novo DSA had significantly worse renal function at 12 and 18m vs. those without DSA. The sub-group of patients with DSA+TCMR had the worst Scr at these time points. Moreover, patients with DSA had significantly worse chronicity (IFTA & IF+i) scores- predominantly due to patients in the DSA+TCMR sub-group (Fig 1A). Patients with DSA+TCMR were significantly younger (P=0.02) and had a higher incidence of DGF (P=0.001) and both were independent risk factors (recipient age OR 0.95, P<0.05; & DGF OR 6.9, P=0.02). MFI levels for the DSA were significantly higher in the DSA+TCMR sub-group (P=0.03). 27/53 patients with de novo DSA, had PBMCs available for analysis. B cell cytokine profiles at 3m were not significantly different in patients with DSA alone vs. those without. However, patients with DSA+TCMR had a significantly lower ratio of IL-10/TNF-a expression (at or prior to the rejection episode) within T1-transitional, transitional, naïve and memory B subsets, compared to those with DSA alone or no DSA, suggesting DSA+TCMR is associated with a pro-inflammatory B cell profile (Fig 1B).
To conclude, de novo DSA with TCMR is associated with renal dysfunction and significantly worse chronic allograft injury than DSA alone. Identifying risk factors (age, DGF, B cell profile) may permit early diagnosis and treatment or prophylaxis with augmented IS.
CITATION INFORMATION: Cherukuri A, Mehta R, Sood P, Zeevi A, Hariharan S, Rothstein D. Early De Novo DSA with T Cell Mediated Rejection (TCMR) Is Associated with Allograft Dysfunction with Chronic Injury. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Cherukuri A, Mehta R, Sood P, Zeevi A, Hariharan S, Rothstein D. Early De Novo DSA with T Cell Mediated Rejection (TCMR) Is Associated with Allograft Dysfunction with Chronic Injury. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/early-de-novo-dsa-with-t-cell-mediated-rejection-tcmr-is-associated-with-allograft-dysfunction-with-chronic-injury/. Accessed February 20, 2026.« Back to 2016 American Transplant Congress
