Zero HLA Mismatch Matters in ABO Incompatible Kidney Transplant.
1Washington University in St. Louis, St. Louis
2Saint Louis University, St. Louis
Meeting: 2017 American Transplant Congress
Abstract number: 56
Keywords: HLA matching, Kidney
Session Information
Session Name: Concurrent Session: Kidney Living Donor Evaluation and Recruitment
Session Type: Concurrent Session
Date: Sunday, April 30, 2017
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:54pm-3:06pm
Presentation Time: 2:54pm-3:06pm
Location: E450a
Transplantation across blood group incompatibilities (ABOi) after preconditioning has emerged as an acceptable option for expanding live donor kidney transplantation (LKDT) to more patients who can benefit compared to dialysis. Data are lacking on the impact of HLA matching on outcomes after ABOi LDKT.
We performed a retrospective analysis of adult (age >18) recipients of ABOi LDKT recorded in the Organ Procurement and Transplantation Network (OPTN) database between 2000 and 2013. ABOi LDKT recipients were categorized into 4 groups according to level of HLA mismatch (HLA MM); 0, 1-3, 4-5, and 6 Associations between HLA MM and posttransplant graft failure and patient death were examined by Cox regression over up to 13 yrs of follow-up.
There were 1,266 ABOi LDKT in the study period. Of these, the distribution of HLA MM was: 0 MM, 7.3%; 1-3 MM, 37.2%; 4-5, 43.2%; 6 MM, 12.32%. Compared to 4-5 HLA MM, recipients with 0 HLA mismatch had a better kidney 10 yr allograft survival [70% vs 49%, adjusted hazard ratio (aHR) 0.52; 95% CI 0.29-0.91]. In contrast, recipients with 1-3 (aHR 0.89; CI 0.69-1.13) and 6 (aHR 0.93; CI 0.64-1.34) HLA MM showed no significant difference in graft survival compared to 4-5 MM. 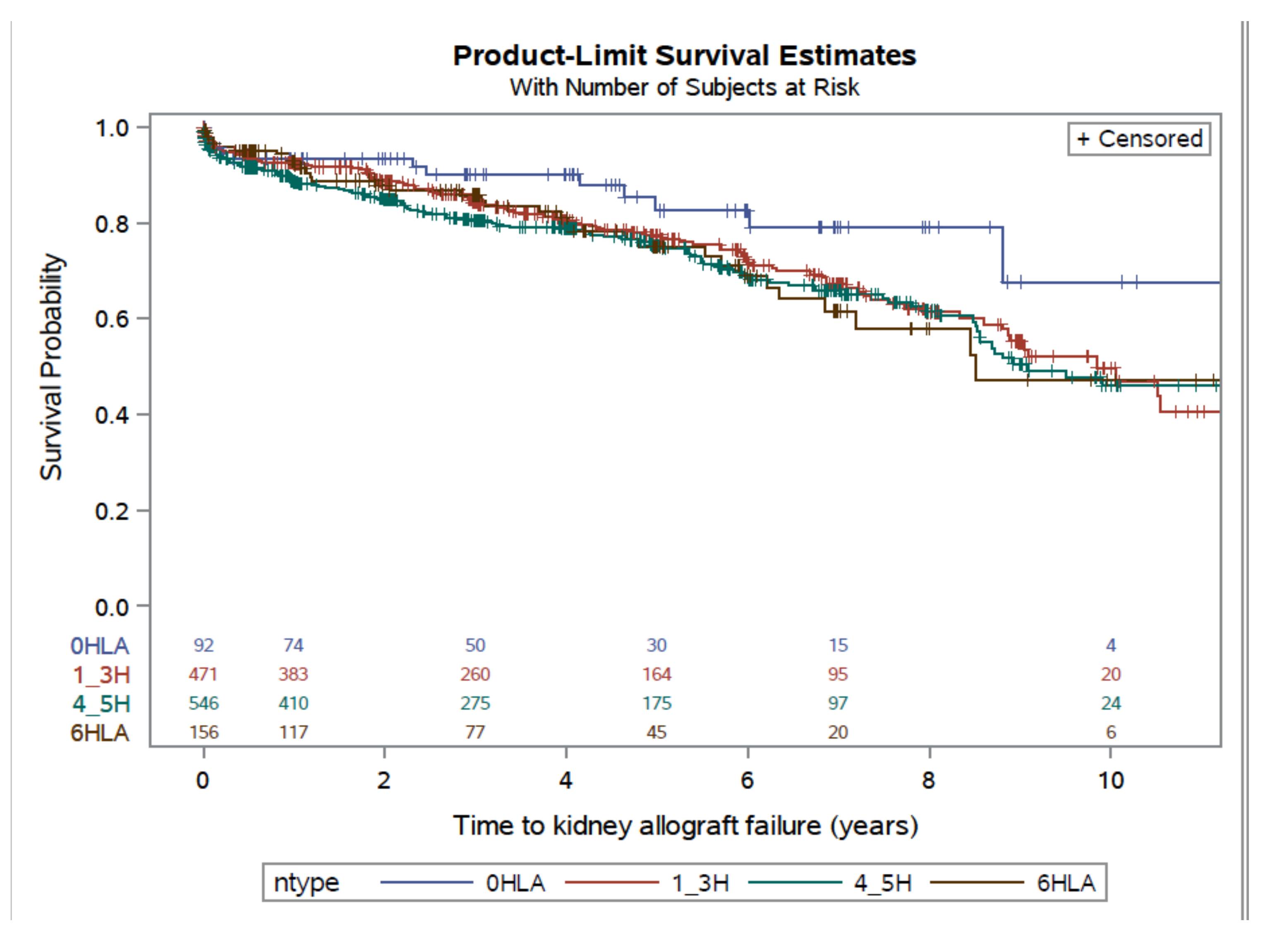 Among recipients of ABOi LDKT, 0 antigen mismatching improves allograft survival compared to 4-5 HLA mismatches. However, in all groups, ABOi LKDT offers an import option to improve survival compared to dialysis.
Among recipients of ABOi LDKT, 0 antigen mismatching improves allograft survival compared to 4-5 HLA mismatches. However, in all groups, ABOi LKDT offers an import option to improve survival compared to dialysis.
CITATION INFORMATION: Alhamad T, Lentine K, Venkatachalam K, Malone A, Brennan D. Zero HLA Mismatch Matters in ABO Incompatible Kidney Transplant. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Alhamad T, Lentine K, Venkatachalam K, Malone A, Brennan D. Zero HLA Mismatch Matters in ABO Incompatible Kidney Transplant. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/zero-hla-mismatch-matters-in-abo-incompatible-kidney-transplant/. Accessed February 20, 2026.« Back to 2017 American Transplant Congress
