Variability in Incidence of Clostridium difficile Infections and Associated Mortality Among Solid Organ Transplant Recipients
Pharmacy, Tampa General Hospital, Tampa, FL.
Meeting: 2015 American Transplant Congress
Abstract number: B25
Keywords: Post-operative complications
Session Information
Session Name: Poster Session B: Bacterial/Fungal/Other Infections
Session Type: Poster Session
Date: Sunday, May 3, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Purpose: Solid organ transplant (SOT) recipients are at risk for Clostridium difficile infection (CDI) due to immunosuppression, frequent healthcare system contact, and liberal use of broad-spectrum anti-infectives and acid suppressants. Given that incidence is expected to vary by organ, we sought to quantify organ-specific rates of CDI and associated mortality in the first post-transplant year.
Methods: An IRB-approved review of adult SOT recipients from 1/2012-1/2013 was conducted to determine 12-month CDI incidence and associated mortality; pertinent demographics and readmission data was collected for the first post-transplant year. All CDI was diagnosed by PCR.
Results: A total of 338 SOT recipients were included; 25 (7.4%) developed CDI within the first post-transplant year. 164 kidney, 93 liver, 46 heart, and 35 lung transplant recipients were included; 12-month incidence of CDI by organ was 3% (5/164), 9.7% (9/93), 10.8% (5/46), and 14.3% (5/35) respectively. CDI was not associated with a statistically significant increase in 1-year mortality (12% vs. 5.75%, p=0.2); mortality was also no different within each organ group (figure 1). Non-renal transplant was associated with significantly higher rates of CDI (11.5% vs. 3%, p=0.003). No baseline demographics appeared to contribute to increased risk of CDI development, save initial transplant length of stay, which was significantly longer for CDI patients compared with non-CDI (12 days vs. 7 days, p=0.018). 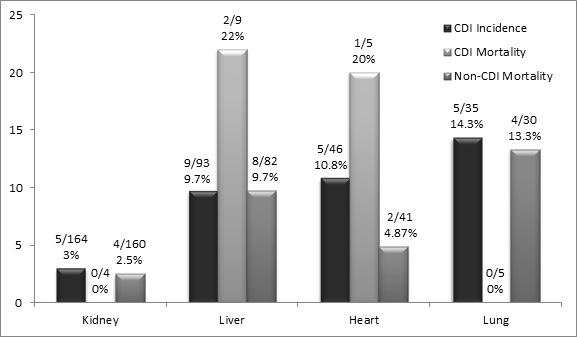
| CDI (n=25) | No CDI (n=313) | P-value | |
| Age, mean | 59.6 | 55.6 | NS |
| Male gender, n (%) | 16 (69.6) | 220 (70) | NS |
| BMI, mean | 26.2 | 27.2 | NS |
| Caucasian race, n (%) | 18 (78.3) | 241 (76.8) | NS |
| GFR at 6 months, mean | 49.95 | 55.36 | 0.09 |
| Initial transplant length of stay in days, median | 12 | 7 | 0.018 |
| Number of readmissions in first 6 months, mean | 0.739 | 0.697 | NS |
Conclusions: CDI is a prevalent nosocomial infection post-transplant, especially in the non-renal transplant population. Prolonged length of stay appears to increase CDI risk. Despite a lack of statistical significance, there was an alarmingly increased rate of mortality in those with CDIs.
To cite this abstract in AMA style:
Piccicacco N, Doligalski C, Logan A. Variability in Incidence of Clostridium difficile Infections and Associated Mortality Among Solid Organ Transplant Recipients [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/variability-in-incidence-of-clostridium-difficile-infections-and-associated-mortality-among-solid-organ-transplant-recipients/. Accessed February 24, 2026.« Back to 2015 American Transplant Congress
