Utilization and Outcomes of Simultaneous Liver-Kidney Transplants after Change in Allocation Policy
1Surgery, Duke University Hospital, Durham, NC, 2Medicine, Duke University Hospital, Durham, NC
Meeting: 2020 American Transplant Congress
Abstract number: 580
Keywords: Allocation, Kidney transplantation, Kidney/liver transplantation, Outcome
Session Information
Session Name: Liver: MELD, Allocation and Donor Issues (DCD/ECD) II
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:15pm-4:27pm
Presentation Time: 4:15pm-4:27pm
Location: Virtual
*Purpose: The July 10, 2017 change in simultaneous liver-kidney (SLK) listing policy imposed more stringent criteria on recipient renal function. Recipient outcomes following this change have not yet been described.
*Methods: We used adult SLK recipients in the UNOS database transplanted 2007-2018. Patients were separated into 3 eras: 2007-2011, 2012- July 10, 2017 (policy change), and July 11, 2017-July 2018. Patient and graft survival was compared at 1 year using Chi-squared test and multivariable Cox proportional hazard models.
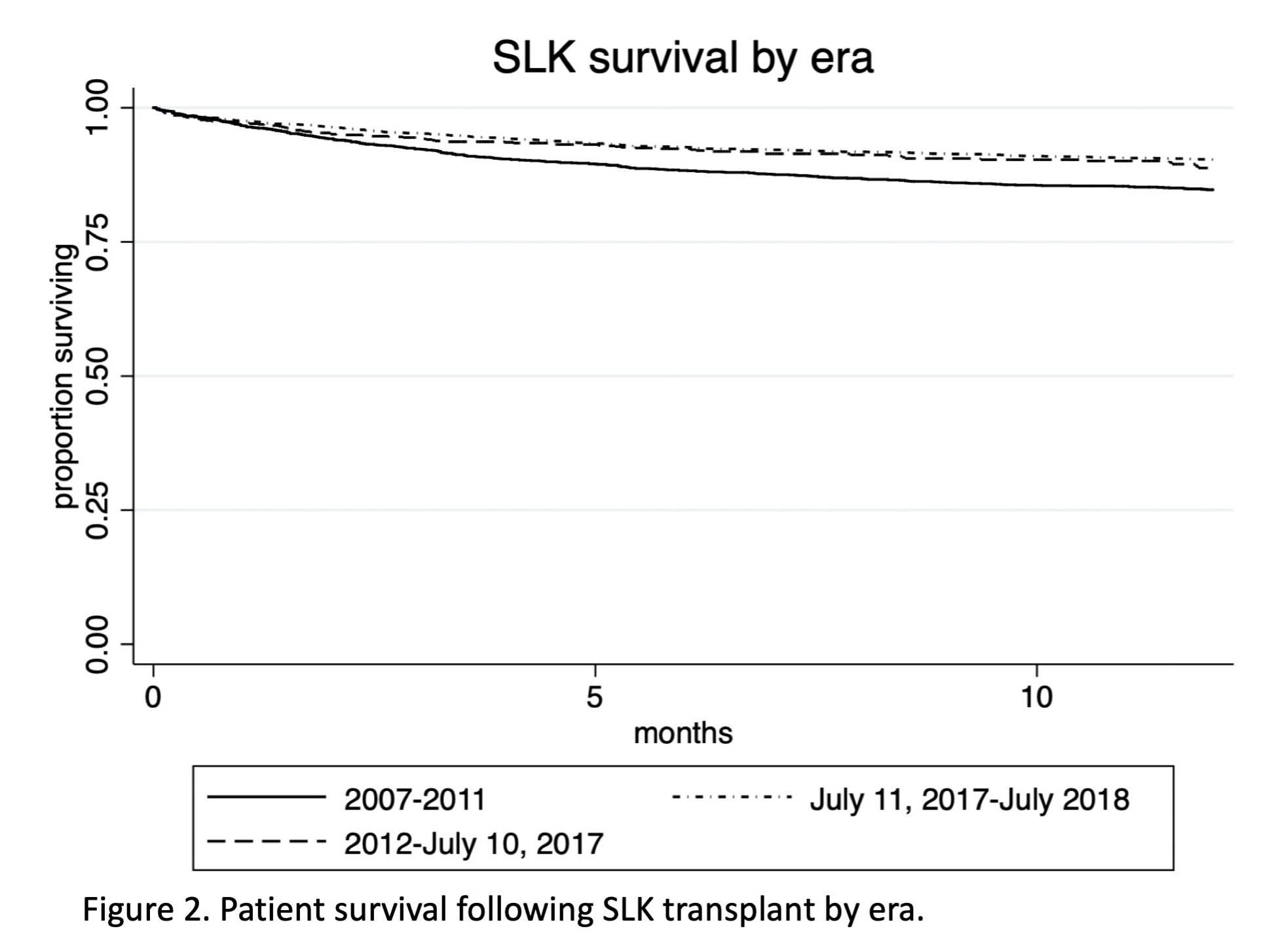
*Results: A total of 5,809 patients received SLKs; 1,892, 3004, and 913 per era, respectively (Figure 1, Table 1). Donor age and KDPI were similar among eras; the number of ECD donors decreased over time (10%, 8%, 7% respectively). The proportion of patients on HD while listed did not change over time (72.5% vs 72.6% vs. 73.0%, p=0.96), nor did the mean GFR at transplant among those not on HD (21.7 vs 21.1 vs 21.2 mL/min, p=0.83). One-year survival improved between the first two eras and remained unchanged after the policy change (85 % vs 90% vs. 91%, p=0.37) (Figure 2). Similar trends were observed for liver and kidney graft survival. Multivariable models demonstrated no difference in survival in the five years pre vs. post-policy (HR 1.24 95% CI 0.96-1.60, p=0.10), but did suggest an increased hazard of liver graft failure within the first year (HR 1.28 95%CI 1.01-1.63, p=0.047).
*Conclusions: Recipient renal function at transplant appears unchanged after the change in SLK listing policy. Despite concern that the policy change would select for sicker recipients and result in poor outcomes, short-term outcomes are similar to prior. Further attention is necessary to the factors affecting outcomes of liver grafts and center-level differences in practice.
| 2007-2011
n=1892
|
2012-July 10, 2017
n=2004
|
July 11, 2017-July 2018
n=913
|
p-value | |
| Donor age, median(IQR) | 35 (23-48) | 33 (24-46) | 34 (24-46) | 0.33 |
| KDRI, median(IQR) | 1.05 (0.88-1.33) | 1.04 (0.87-1.29) | 1.05 (0.88-1.31) | 0.01 |
| Recipient age (median, IQR) | 56 (50-61) | 58 (51-63) | 58 (51-63) | <0.0005 |
| Diagnosis, n(%)
HCV
EtOH
NASH
HCC
|
492 (28%)
81 (5%)
183 (10%)
172 (10%)
|
639 (22%)
699 (24%)
498 (17%)
302 (10%)
|
120 (13%)
249 (28%)
194 (22%)
80 (9%)
|
<0.0005 |
| Recipient BMI >= 35 | 198 (10%) | 332 (18%) | 115 (13%) | 0.092 |
| HD while on waitlist | 1371 (72%) | 2180 (73%) | 666 (73%) | 0.96 |
To cite this abstract in AMA style:
Samoylova ML, Shaw BI, Kesseli SJ, Sanoff S, Patel Y, Barbas AS, McElroy L. Utilization and Outcomes of Simultaneous Liver-Kidney Transplants after Change in Allocation Policy [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/utilization-and-outcomes-of-simultaneous-liver-kidney-transplants-after-change-in-allocation-policy/. Accessed March 6, 2026.« Back to 2020 American Transplant Congress