Use of Continuous Glucose Monitoring (CGM) in the Evaluation of Auto-Islet Candidates
Surgery, University of Arizona, Tucson, AZ
Meeting: 2013 American Transplant Congress
Abstract number: D1579
Purpose: We used continuous glucose monitoring (CGM) as a comparative tool with glycated hemoglobin A1c (HbA1c) to assess metabolic function in auto-islet transplant candidates.
Methods: From April 2010 to November 2012, 36 auto-islet candidates underwent 5 day CGM during their transplant evaluation; CGM results were correlated with results from HbA1c (P < 0.01). CGM measurements were obtained to calculate the percent time a subject's glucose values were above the normal upper (> 120 mg/dl) and lower (< 65 mg/dl) limit for interstitial fluid glucose, along with the average glucose level.
Results: 36 (23F/13M) auto islet candidates were evaluated. The mean and median age were 39 years (range 20 – 66 years), mean BMI was 26.2 (median 26; range 16.9 – 46.6). All candidates pre-transplant HbA1c values were normal (< 6.4%); the mean and median pre-transplant HbA1c were 5.6% (range 4.6 – 6.3%). Only 13 candidates experienced hypoglycemic episodes as measured by pre-transplant CGM; 3 (8%) of candidates experienced hypoglycemia for more than 5% of the CGM evaluation period (range 1 – 7% of time below normal glucose limit). Four candidates’ CGM results were normal as defined by glucose levels within normal glycemic ranges for at least 96% of the time; 89% of patients experienced abnormal CGM measurements despite normal baseline HbA1c results. Figure 1 shows the distribution between relative duration above 120 mg/dL and HbA1c results for auto-islet candidates.
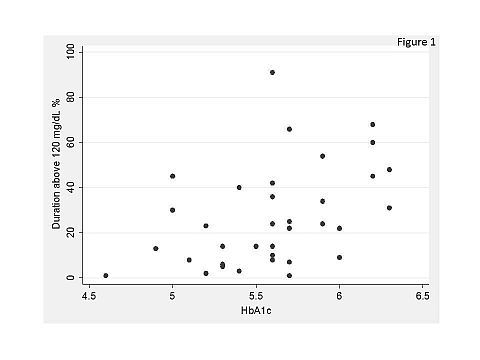
Conclusion: All patients presented with normal pre-transplant HbA1c levels despite evidence of diminished pancreatic function using CGM. HbA1c is a common assessment tool used to determine pre-transplant metabolic function but may not provide the most complete picture of the degree of glycemic control in this patient cohort. Further investigation with a larger study sample size is needed to validate these correlations and to see if CGM correlates with post-transplant outcomes such as insulin requirements. In conclusion, using CGM in tandem with HbA1c can be useful in the assessment of B-cell function in auto-islet transplant candidates.
To cite this abstract in AMA style:
Rilo H, Delbridge M, Grigsby B, Rana A, Porubsky M, Gruessner A, Gruessner R. Use of Continuous Glucose Monitoring (CGM) in the Evaluation of Auto-Islet Candidates [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/use-of-continuous-glucose-monitoring-cgm-in-the-evaluation-of-auto-islet-candidates/. Accessed February 27, 2026.« Back to 2013 American Transplant Congress
