Urinary Protein Excretion in Non-Renal Transplant Patients – Does mTOR-Inhibitor Treatment Matter?
The H2304 Study Group, Basel, Switzerland
Meeting: 2013 American Transplant Congress
Abstract number: D1695
Background
The interplay of glomerular filtration and tubular absorption of proteins with various molecular weights defines the pattern and magnitude of daily urinary protein excretion (UPE). Increased UPE, also referred to as proteinuria, serves as a clinical surrogate marker for renal injury and progressive damage in a variety of diseases affecting different parts of the nephron. mTOR-inhibitor treatment has also been associated with increased UPE not only in KTx but also non-renal Tx recipients.
Method
Data were retrieved from study H2304 (NCT00622869), a 24-month(M), randomized, multicenter study in 719 de novo LTx recipients comparing everolimus (EVR, C0 3-8 ng/mL) plus reduced tacrolimus (TAC, C0 3-5 ng/mL) to standard TAC (TAC-C, C0 6-10 ng/mL). Here, the total daily UPE, measured as urinary protein-to-creatinine ratio, as well as a set of differently sized urinary proteins will be described in order to allow a more detailed investigation of the origin and course of UPE in de novo LTx patients receiving EVR.
Results
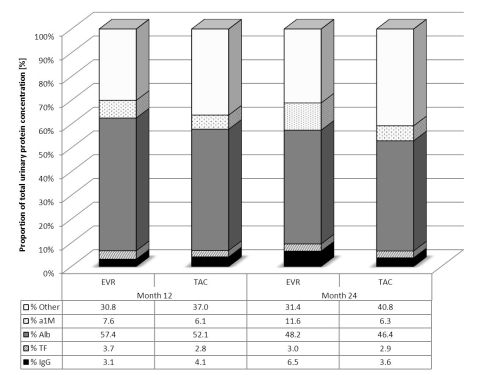
UPE was higher with EVR plus reduced TAC compared to standard TAC with highest values at M6 (290 mg/day) followed by decreasing values at M12 and a further decrease to 194 mg/day at M24. Daily UPE maintained stable in TAC Control at 158 mg/day. UPE ≥500 mg/day at any time point occurred in 18.1% of patients in TAC-C vs. 23.6% in EVR+rTAC (18.9% when EVR C0 was in the range of 3-8 ng/mL). Analysis of urinary protein electrophoresis determining the distribution pattern of alpha 1 microglobulin (26 kDa), albumin (70 kDa), transferrin (80 kDa), and immunoglobulin G (150 kDa) are shown in Fig1 demonstrating similar patterns for EVR and TAC.
Discussion
Clinical observations suggest that mTOR-inhibitor treatment might be associated with increased UPE, potentially due to enhanced cell wall permeability and podocyte dysregulation. However, in case of mTOR-inhibitor facilitated reduction of CNI exposure, the improvement in glomerular blood flow and consequently a higher overall protein filtration in combination with mTOR-dependent reduction in tubular protein reabsorption may also contribute to increased urinary protein excretion without pathological significance.
Junge, G.: Other, NVS, H2304 Study Group. De Simone, P.: Other, NVS, H2304 Study Group. Fung, J.: Other, NVS, H2304 Study Group. Kohler, S.: Other, NVS, H2304 Study Group. Saliba, F.: Other, NVS, H2304 Study Group.
To cite this abstract in AMA style:
Junge G, Simone PDe, Fung J, Kohler S, Saliba F. Urinary Protein Excretion in Non-Renal Transplant Patients – Does mTOR-Inhibitor Treatment Matter? [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/urinary-protein-excretion-in-non-renal-transplant-patients-does-mtor-inhibitor-treatment-matter/. Accessed February 28, 2026.« Back to 2013 American Transplant Congress
