Transplant Center Effect on Acute Liver Failure Outcomes in a National Cohort
University of Pennsylvania, Philadelphia, PA
Meeting: 2020 American Transplant Congress
Abstract number: C-162
Keywords: Allocation, Liver failure, Survival, Waiting lists
Session Information
Session Name: Poster Session C: Liver: Recipient Selection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Transplant centers coordinate complex care for patients with acute liver failure (ALF), in whom liver transplantation (LT) can be lifesaving. This study examines associations between transplant center characteristics and ALF waitlist outcomes.
*Methods: This retrospective cohort study included adults with ALF listed for LT between 2002-2019 within the United Network for Organ Sharing database. Transplant centers were divided into tertiles of ALF volume (low: <20; medium: 20-39; high: 40+ ALF listings during the study period) and total LT volume (low: <600; medium: 600-1199; high: 1200+ LTs during the study period). Multinomial regression was used to obtain predicted probabilities of each waitlist outcome (LT, died/too sick, spontaneous survival [SS]) at the recipient level adjusted for clinical characteristics. Estimates were then used to obtain center-level observed-to-expected ratios for each outcome.
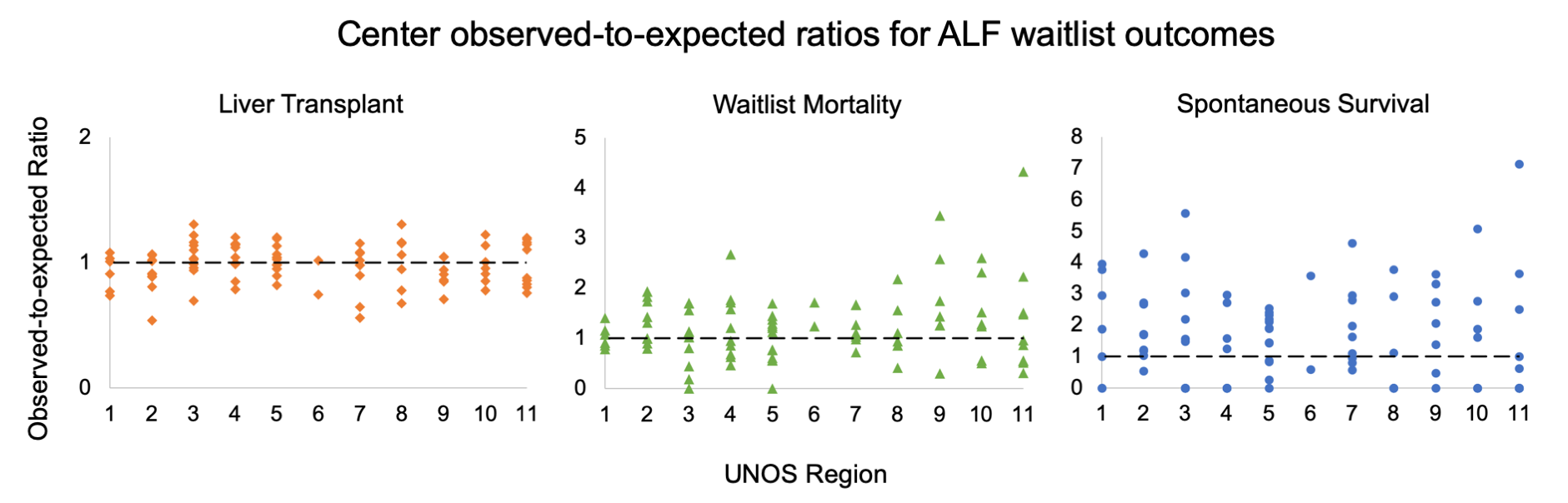
*Results: 3,248 ALF patients were waitlisted at 92 centers. The median rates of each outcome by center were: 72.6% LT (interquartile range [IQR] 65%-81%), 18.2% died/too sick (IQR: 12.7-22.8%), and 6.1% SS (IQR: 0-11.5%). ALF volume was not associated with LT or waitlist mortality rates (p=0.8, p=0.2 respectively). However, ALF volume was significantly associated with SS: median 0% for low-volume (IQR: 0-0.09%), 5.9% for medium-volume (IQR: 0-13.6%), and 8.6% for high-volume ALF centers (IQR: 3.2-11.5%; p=0.039). In contrast, overall LT volume was associated with waitlist mortality for ALF, where low-volume LT centers had the highest mortality rates (median 21.4%, IQR: 16.1-26.7%; p=0.042). LT volume was not significantly associated with SS or LT rates (p=0.1 for both outcomes). Center observed-to-expected ratios for each outcome showed no geographic trends, though outliers in both under- and over-performance were apparent (Figure). The greatest variation across centers was seen for SS, which ranged from 0 at 28 centers to >4 at 6 centers.
*Conclusions: High ALF volume is associated with greater SS rates, and low LT volume with greater waitlist mortality. Significant heterogeneity was seen across centers in ALF waitlist mortality and SS rates, despite adjusting for differences in patient case-mix and severity of illness.
To cite this abstract in AMA style:
Wong NZ, Reddy KR, Bittermann T. Transplant Center Effect on Acute Liver Failure Outcomes in a National Cohort [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/transplant-center-effect-on-acute-liver-failure-outcomes-in-a-national-cohort/. Accessed February 17, 2026.« Back to 2020 American Transplant Congress