Titer Stability vs. Terminal Pre-transplant Titer: Titer History is Irrelevant for A2 to B Transplantation
1Medstar Georgetown Transplant Institute, Washington, DC, 2Johns Hopkins Medical Center, Baltimore, MD
Meeting: 2021 American Transplant Congress
Abstract number: 827
Keywords: Allocation, Outcome, Rejection
Topic: Clinical Science » Kidney » Kidney Deceased Donor Allocation
Session Information
Session Name: Kidney Deceased Donor Allocation
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Minor ABO incompatibile (ABOi) transplants from blood group A2 or A2B donors have increased since 2014, but initial guidance suggested that establishing an anti-A titer history is critical for effective transplantation. We reviewed our center’s data to determine the relevance of the anti-A titer history in transplant outcomes.
*Methods: This is a retrospective study. We reviewed all patients who received kidneys across minor ABOi. All patients getting minor ABOi transplants received standard treatment without any additional plasmapheresis. Recipients were categorized as those with only a single titer measurement pre-transplant vs those who had a titer history with readings over at least 3 months. For those with a titer history, we further stratified patients into those with persistently low titers (less than 1:8) and those that had at least 1 high titer but whose titers returned to low levels prior to being transplanted. The outcome of rejection or graft loss was evaluated using Kaplan-Meier plots and analyzed with the Mantel-Cox log rank test.
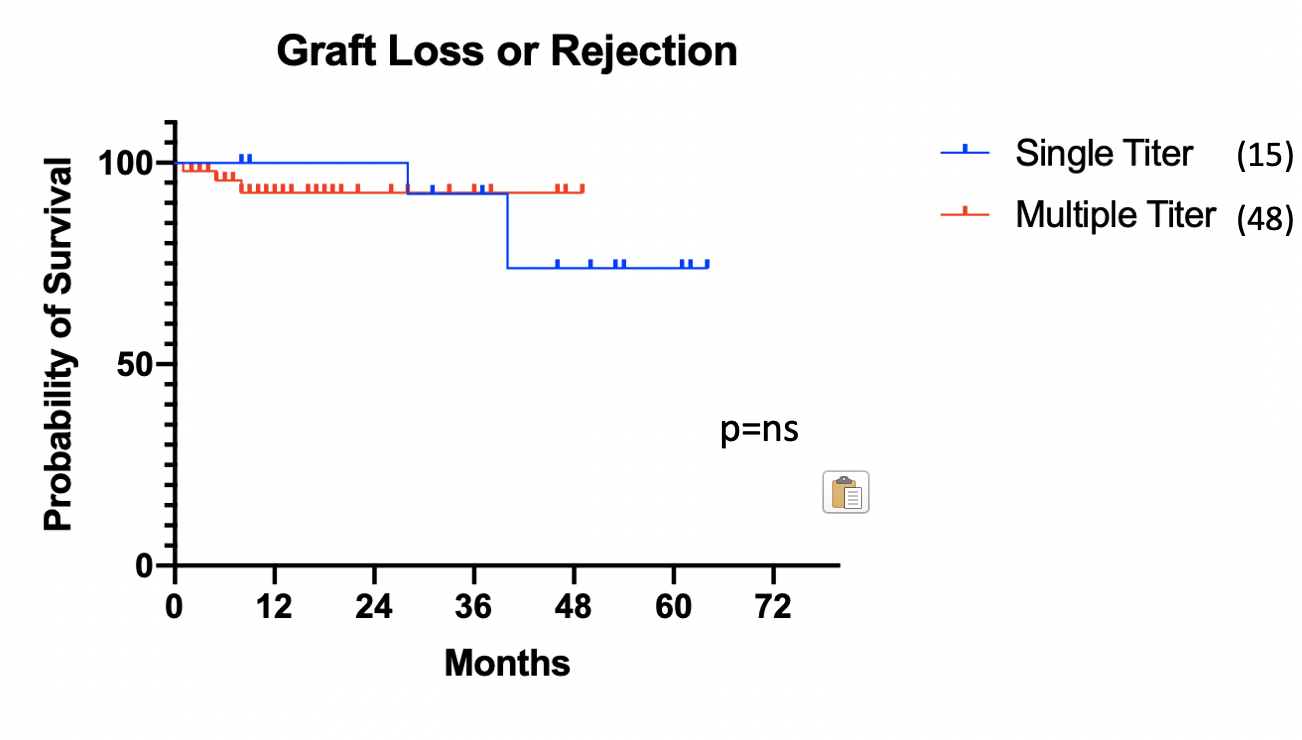
*Results: Among our minor ABOi recipients, we found 15 had only a single anti-A titer and 48 had at least a 3 month titer history. We also identified 46 recipients who were transplanted with persistently low titers compared with 13 who had been identified with one or more high titers that returned to low levels by the time of transplant. Kaplan-Meier analysis showed no advantage in having an extended titer history (figure 1). Mean creatinine at 3 months and 1 year were not statistically different between the groups (1.55 vs 1.54 at 3m p=0.96, 1.57 vs 1.51 at 1 yr p=0.75).
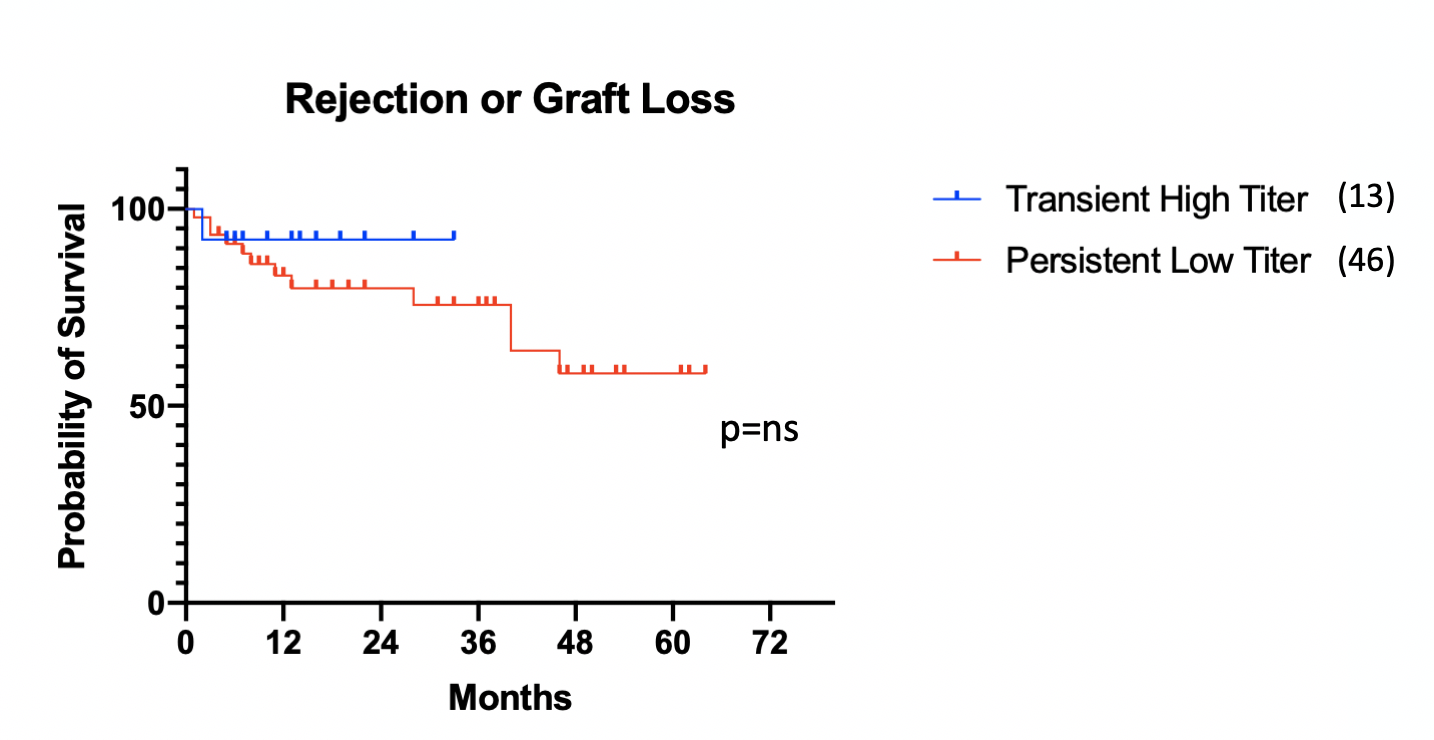
Similarly, in those with a history, a prior high titer that resolved before transplantation was associated with no increased incidence of graft loss or rejection (figure 2). Mean creatinine at 3m and 1yr were statistically similar (1.86 vs 1.50 at 3m p=0.10, 1.57 vs 1.43 at 1yr, p=0.53)
*Conclusions: Contrary to common practice, a recipient’s anti-A titer history demonstrated no significance in predicting graft outcomes as long as the titers were low at the time of transplant. Transplantation across minor ABOi does not require a titer history to be safe and effective.
To cite this abstract in AMA style:
Gilbert A, Radomski S, Vucci J, Thomas B, Cooper M. Titer Stability vs. Terminal Pre-transplant Titer: Titer History is Irrelevant for A2 to B Transplantation [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/titer-stability-vs-terminal-pre-transplant-titer-titer-history-is-irrelevant-for-a2-to-b-transplantation/. Accessed March 7, 2026.« Back to 2021 American Transplant Congress